 |
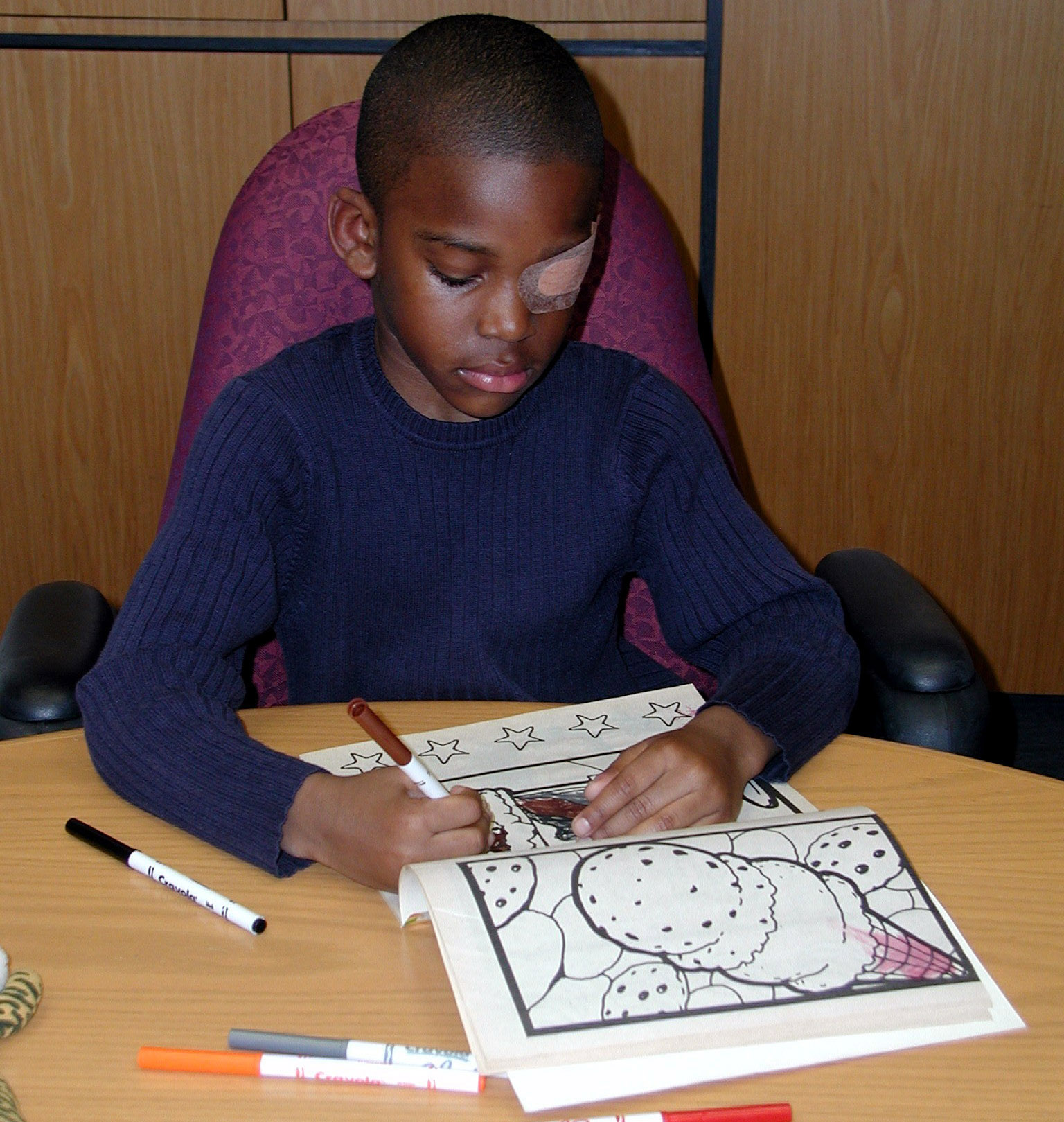
| Treatments that were combined and developed through computer games received a more enthusiastic response from the children than patching alone, perhaps lending to greater compliance. Photo: National Eye Institute/NIH. Click image to enlarge. |
Three different treatments were recently investigated by Spanish researchers in terms of efficacy for improvements in children with amblyopia. Currently, active vision therapy for the condition demonstrates good results; however, there is no standard protocol for vision therapy, thus prompting them to investigate further.
The three treatments included two protocols combining patching with vision therapy and one with patching alone. Of the two protocols, the first included perceptual learning with a computer game, designed to favor medium-to-high spatial frequency achromatic mechanisms of parvocellular origin; the second involved vision therapy with a specific protocol and two-hour patching. A total of 52 amblyopic kids aged four to 12 were randomly assigned to the three groups: (1) two-hour patching, (2) monocular perceptual learning and (3) two-hour patching plus vision therapy. After three months, visual outcomes were assessed and compared with a control group of 36 patients with normal vision.
Positively, it was found that visual acuity (VA) and stereoacuity improved after treatment in all three groups; however, the best results occurred in those who had patching plus VT, followed by those who had patching plus monocular perceptual learning—patching alone was the least effective. Change in interocular VA difference was significant for monocular perceptual learning, then patching. Stereoacuity differences between groups were not observed. Final outcomes of VA and interocular differences were influenced by baseline VA and interocular difference, respectively, with greater improvement in those with poorer initial values.
Generally speaking, the authors relay that “these results suggest that vision therapy should include monocular accommodative exercises, ocular motility and central fixation exercises where the fovea is more active.”
The authors further discuss how a neuronal model suggests that perceptual learning strengthens direct feeding connectivity between the lateral geniculate nucleus and V1. If this is the case, it’s possible learning occurred before binocular signals were combined in a way that was specific to the trained eye and contributed to binocular combination. As they then explain, “therefore, increasing the use of monocular perceptual learning tasks in a clinical setting may be beneficial before moving on to binocular tasks or even performing them at the same time. Thus, this option may be more practical than prolonged occlusion, where the amblyopic eye is more passive.”
From their findings, the researchers clinically suggest that “both monocular perceptual learning and patching plus vision therapy as a treatment paradigm in severe amblyopia to shorten the duration of occlusion prior to binocular treatment. This would avoid, at least in part, the negative effects of patching on the visual system and on the child’s psychosocial well-being and self-esteem.”
| Click here for journal source. |
Hernández-Andrés R, Serrano MÁ, Alacreu-Crespo A, Luque MJ. Randomised trial of three treatments for amblyopia: vision therapy and patching, perceptual learning and patching alone. Ophthalmic Physiol Opt. October 12, 2024. [Epub ahead of print]. |