The When and Why of Ordering Blood Work
This is within most OD’s scope of practice—don’t be afraid to use it.
By Blair Lonsberry, MS, OD, MEd
Release Date: February 21 2018
Expiration Date: February 21, 2021
Goal Statement: Many ocular conditions have a systemic etiology diagnosed with lab testing. Whether ordering lab tests independently or comanaging with a primary care provider, optometrists must have a working knowledge of what tests to order and what the results mean. This article discusses the common lab tests necessary to diagnose systemic conditions such as diabetes, liver and kidney diseases, systemic inflammatory diseases, autoimmune disorders and infectious diseases.
Faculty/Editorial Board: Blair Lonsberry, MS, OD, MEd
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 56820-PD. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Authors: The author has a financial relationship with Alcon, Carl Zeiss Meditec, Optovue, Shire and Sun Pharmaceuticals.
Editorial staff: Jack Persico, Rebecca Hepp, William Kekevian, Michael Iannucci and Francesca Crozier-Fitzgerald all have no relationships to disclose.
As optometry continues to expand its therapeutic privileges, the OD’s role in the diagnosis, management and prevention of systemic health conditions is more important than ever—and an integral part in the diagnosis is lab testing. Regardless of whether the optometrist is ordering lab tests independently or is comanaging with a primary care provider (PCP), a working knowledge of what tests to order and what the results mean is crucial.
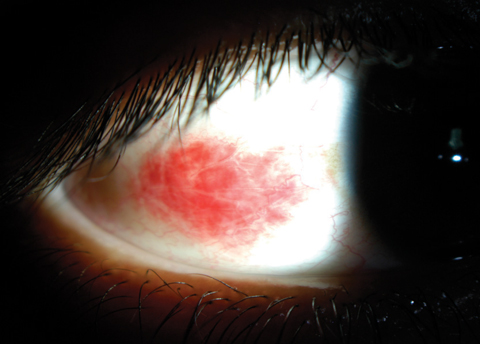 |
| Fig. 1. Subconjunctival hemorrhage may be an indication of underlying anemia, which would require a CBC to hone in on the diagnosis. |
Testing Basics
Most lab tests require a blood draw. Some require a urine sample, such as the nucleic acid amplification test (NAAT) for chlamydia and gonorrhea, or swab testing (oral and anal chlamydia/gonorrhea cannot be diagnosed from urine sample and require oral/anal swabs).1 All of these require the patient get the testing done at an accredited facility. Some have specific pretest requirements such as fasting (e.g., fasting plasma glucose, lipid panel) or can be influenced by pretest conditions (e.g., patient hydration levels and excessive meat intake can alter kidney function tests), and it is important to educate the patient prior to sending them to the lab.2
Laboratory reports typically include when the sample was collected, when it was analyzed and the name of the person who requested the testing. The results will include a set of reference ranges for each test that are based on “normal” values for the average population and may be further classified by other variables such as race, age and gender. Any result that falls outside of the reference range is typically highlighted in some fashion (Table 1).3,4
A complete blood count with differential (CBC with diff) is probably one of the most common blood tests ordered and can often help to explain patient symptoms such as weakness, fatigue or bruising.3,5 A CBC provides important information about the kinds and numbers of cells in the blood, especially red and white blood cells and platelets (Table 2).
| Table 1. Kidney Function Test Results | |||
| Component | Your Value | Standard Value | Flag |
| Creatinine | 1.35mg/dL | .06mg/dL to 1.3mg/dL | H |
| GFR Afr Amer(CKD-EPI) | 70mg/dL | ≥60mg/dL | |
| GFR nonAfr Amer(CKD-EPI) | 61mg/dL | ≥60mg/dL | |
| This common kidney function testing report includes the patient’s creatinine and glomerular filtration rate (GFR). The creatinine levels are slightly elevated, highlighted by the “H” in the furthest column. | |||
A CBC with diff may be ordered for a variety of conditions that have associated ocular manifestations such as anemia, leukemia, infections or recurrent inflammation. Patients who have recurrent subconjunctival hemorrhages may have underlying anemia and would require a CBC to help rule it out (Figure 1).4 A CBC may be ordered in a patient who presents with a bilateral uveitis to rule out the possibility of a systemic infection (e.g., elevated white blood count may be an indication of a bacterial infection). A CBC should also be ordered for patients who have unexplained retinal hemorrhages, cotton wool spots or both. Patients prescribed certain medications, such as oral steroids, blood thinners and diuretics, should have baseline testing and periodic monitoring.3,4
Lipid testing is often ordered as part of “routine” lab testing but is particularly important in patients with diabetes and for assessing risk for cardiovascular disease.3,6 The American Association of Clinical Endocrinologists published 2017 guidelines for the management of dyslipidemia and prevention of cardiovascular disease, and have included a new “extreme risk” group.6
Patients who have arcus at a younger age (arcus juvenilis) or Hollenhorst plaques should have their cholesterol levels evaluated.4 There are several specific components of cholesterol evaluation (Table 3):3
Total cholesterol. This measures all of the cholesterol in all the lipoprotein particles.
High-density lipoprotein cholesterol (HDL-C). This measures the cholesterol in HDL particles; often called “good cholesterol” because it removes excess cholesterol and carries it to the liver for removal.
Low-density lipoprotein cholesterol (LDL-C). This calculates the cholesterol in LDL particles; often called “bad cholesterol” because it deposits excess cholesterol in walls of blood vessels, which can contribute to atherosclerosis. Usually, the amount of LDL-C is calculated using the results of total cholesterol, HDL-C and triglycerides.
Triglycerides. This test measures all the triglycerides in all the lipoprotein particles; most is in the very low-density lipoproteins.3
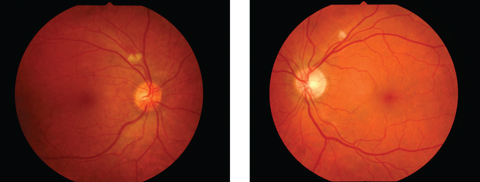 |
| Fig. 2. This cotton wool spot superior to the optic nerve in the right and left eye of a 38-year-old asymptomatic female patient led us to order testing, which revealed a diagnosis of anemia. Click images to enlarge. |
Case Example:
A 38-year-old white female presented for an updated spectacle correction. Her medical history was negative, she was taking birth control and a multivitamin, she denied any history of smoking and is an occasional alcohol consumer. Visual acuities (VAs) were correctable to 20/20 in both eyes, entrance skills were unremarkable, slit lamp was unremarkable and intraocular pressures (IOPs) were 16mm Hg OD and OS.
Upon dilated fundus exam, a cotton wool spot was noted in both eyes (Figure 2). Blood pressure measured 125/82mm Hg. She was referred to her PCP, who found her blood glucose and glycosylated hemoglobin test (A1c) values were normal and repeat blood pressure evaluation was within the normal range. A CBC with diff ultimately indicated low levels of hemoglobin and hematocrit, and she was diagnosed with anemia.
Here is a look at other common lab tests ODs can order, and how to interpret the results.
| Table 2. Representative CBC with Differential Report with Associated Standard Ranges | |||
| Component | Your Value | Standard Range | Flag |
| WCB | 4.4x10(9)/L | 4.0x10(9)/L to 10.5x10(9)/L | |
| RBC | 5.12x10(12)/L | 4.00x10(12)/L to 5.50x10(12)/L | |
| Hemoglobin | 15.4gm/dL | 13.0gm/dL to 17.0gm/dL | |
| Hematocrit | 46.7% | 37.0% to 50.0% | |
| MCV | 91.2fL | 82.0fL to 100.0fL | |
| MCH | 30.1pg | 28.0pg to 35.0pg | |
| MCHC | 33.0 | 31.0 to 36.5 | |
| RDW, CV | 13.2% | 11.0% to 14.5% | |
| RDW, SD | 44.5fL | 36.0fL to 50.0fL | |
| Platelet count | 223x10(9)/L | 140x10(9)/L to 375x10(9)/L | |
| MPV | 9.6fL | - | |
| This is an example of a CBC with differential lab report. The components of a typical CBC with diff include: Red blood cell count (RBC). This is the total number of RBCs in a specific volume of blood. This value does not give any indication of how the RBCs are functioning, just the total number. Low numbers could be an indication of blood loss, hemorrhaging and certain cancers. High levels could be an indication of time spent in high altitudes, pulmonary fibrosis or dehydration.3,5 Hemoglobin. This represents the amount of oxygen-carrying protein (hemoglobin) in a sample and reflects the number of RBCs present. This is used to screen patients for anemia and other conditions that can result in RBC breakdown. Low Hb levels may indicate anemia, blood loss or deficient levels of vitamin B6 or B12. High levels maybe an indication of sickle cell disease, high altitude or dehydration.3,5 Hematocrit. This value is related to the percentage of total blood volume comprised of RBCs. It is closely related to hemoglobin levels. Low levels can be an indication of anemia, blood loss, certain cancers or vitamin B6 or B12 deficiencies. Elevated levels can be an indication of high altitude or dehydration.3,5 Red blood cell indices. This includes mean corpuscular value (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC) and RBC distribution width (RDW). These indices provide information such as RBC size, weight and hemoglobin concentration and are helpful in classifying anemias. Low values could be an indication of iron deficiency, microcytic anemia or thalassemia. Elevated levels may indicate folic acid or vitamin B12 deficiency, alcohol abuse or macrocytic anemia.3,5 White blood cell count (WBC) and differential. This reflects the number of WBCs per volume of blood. The differential provides detailed information about the types of WBCs (e.g., neutrophils, eosinophils, lymphocytes) present, along with percentages. Low levels may be an indication of autoimmune diseases, liver or spleen disease, radiation sickness or bone marrow dysfunction. Elevated levels maybe present in infectious diseases (bacterial, viral or protozoan), inflammatory conditions, leukemia or severe emotional/physical stress.3,5 Platelet count. This value represents the number of platelets per volume of blood and is useful in diagnosing and managing blood clotting disorders and other diseases. Low values may be an indication of conditions such as leukemia, chemotherapy, hemolytic anemia or vitamin B12 or folate deficiency. Elevated levels maybe present in conditions such as rheumatoid arthritis or certain malignancies.3,5 | |||
Diabetes
This condition is a growing epidemic with significant physical, emotional and economic ramifications. Patients with diabetes should have yearly eye exams to assess for any ocular manifestations of the disease. However, with a large number of undiagnosed patients, it is not uncommon for an eye examination to be the first indication of a patient having diabetes.4,7
Diabetes is primarily diagnosed based on plasma glucose testing. Three main blood glucose tests exist (Table 4):
Fasting plasma glucose (FPG). This is the plasma glucose levels in the blood after the patient has refrained from eating or drinking anything but water for eight hours.8
Glycosylated hemoglobin test (A1c). This reflects the percentage of free glucose bound to hemoglobin in RBCs over a three-month time span. It is important to remember that A1c is an indirect measure of a patient’s average blood glucose levels. Clinicians should consider additional tests when diagnosing diabetes. The National Health and Nutrition Examination Survey data determined that the accepted A1c cut-off of >6.5% (48mmol/mol) identifies one-third fewer cases of undiagnosed diabetes than a fasting glucose cut-off point of >126mg/dL (7.0mmol/L).8
Oral glucose tolerance test (OGTT). This tests the patient’s blood glucose levels before and two hours after drinking 75g of anhydrous glucose dissolved in water. This test is often done at the same time as FPG. The FPG level is the pre-test glucose level and the OGTT value is two hours after drinking the glucose solution. An OGTT test of >200mg/dL (11.1mmol/L) is considered abnormal.8
All three tests are thought to be equally appropriate for diagnostic testing, but a combination of A1c with either a FPG or OGTT results in a more accurate diagnosis.8 The 2017 American Diabetes Association Standards for Diabetes Care recommends clinicians consider testing for Type 2 diabetes in asymptomatic adults of any age who are overweight (BMI >25kg/m2 or >23kg/m2 in Asian Americans) and who have one or more additional risk factors for diabetes.8 In addition, screening should begin for all patients at age 45 and, if tests are normal, repeated at a minimum of three-year intervals. Patients who are suspicious for diabetes or have been diagnosed can benefit from further recommended testing, including:8
- fasting lipid profile
- liver function tests
- urinary albumin-to-creatinine ratio
- serum creatinine and estimated glomerular filtration rate
- thyroid stimulating hormone (TSH) levels in Type 1 diabetes
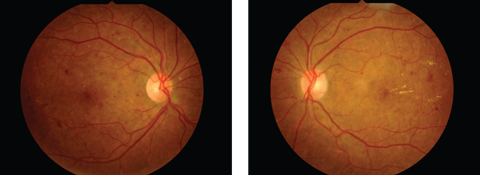 |
| Fig. 3. This 56-year-old male’s fundus images indicate the presence of hemorrhaging and exudates associated with diabetic retinopathy. Click images to enlarge. |
Case Example:
A 56-year-old white patient presented as a walk-in because he broke his current pair of glasses. He was a long-haul truck driver from out of state and needed a new pair of glasses as quickly as possible. His medical history was negative and he wasn’t taking any medications. He was a pack-a-day smoker and occasionally consumed alcohol. His uncorrected VAs were 20/50 OD and 20/40 OS. Entrance skills were unremarkable, manifest refraction revealed +2.25 –0.50 x 180 (20/20) OD and +2.00 DS (20/20) OS. Slit lamp results showed arcus 360 degrees in both eyes. IOPs were 16mm Hg and 17mm Hg. Blood pressure was 125/85mm Hg. Undilated fundus evaluation revealed scattered dot and blot hemes/exudate—prompting dilation (Figure 3).
I told the patient that I didn’t remember him mentioning that he had diabetes. He said he doesn’t, though his wife does. I educated him on the present signs of changes to the back of his eye consistent with diabetes and recommend he see his PCP as soon as possible, as blood glucose testing was not available at this office.
| Table 3. A Representative Lipid Profile | ||
| Component | Your Value | Standard Range |
| Cholesterol | 201mg/dL | ≤239mg/dL |
| Triglyceride | 99mg/dL | ≤199mg/dL |
| HDL Chol | 39mg/dL | ≥40mg/dL |
| LDL Calc | 142mg/dL | ≤159mg/dL |
Two hours later, I received a call from an emergency room physician wanting to discuss the patient. The physician wanted to know why I told the patient he needed to have his blood pressure checked when it is normal. I clarified that I was concerned about his blood sugar, not blood pressure, as I had a strong suspicion that he has diabetes, given my findings of retinal hemorrhages and exudate. The physician wasn’t convinced, but agreed to check his blood glucose levels.
The patient called me two days later and stated that the ER doctor confirmed that he had diabetes with a random plasma glucose level of 380mg/dL and an A1c value of 10.2.
Liver and Kidney Testing
These labs are ordered for a variety of systemic conditions such as diabetes, autoimmune diseases and sarcoidosis—many of which have ocular manifestations. Liver and kidney testing may also be requested in patients taking certain medications, including oral antivirals for prophylaxis of herpes simplex virus, herpes simplex zoster or both.
| Table 4. Criteria for Pre-diabetes and Diabetes Testing8 | ||
| Pre-diabetes | Diabetes | |
| FPG | 100mg/dL to 125mg/dL (5.6mmol/L to 6.9mmol/L) | >126mg/dL (7.0mmol/L) |
| OGTT | 140mg/dL to 199mg/dL (7.8mmol/L to 11.0mmol/L) | >200mg/dL (11.1mmol/L) |
| A1c | 5.7% to 6.4% | >6.5% |
Kidney function tests. Three main tests are common to test kidney function (Table 1). Blood urea nitrogen (BUN) measures the amount of urea nitrogen in the blood, which becomes elevated in patients with kidney dysfunction. A markedly increased BUN is conclusive evidence of severe impaired glomerular function.3,4 Creatinine is produced at a constant rate depending on a person’s muscle mass and is removed from the body by the kidneys. Production of creatinine is constant as long as muscle mass remains constant and reflects renal function. Abnormal elevations as measured by serum creatinine testing indicate renal function impairment.3 The glomerular filtration rate estimates the amount of blood that passes through the glomeruli each minute and provides a good indication of kidney function (and possible staging of kidney disease).3
Liver function tests. Alanine aminotransferase (ALT) is an enzyme found in the liver in high concentrations and relatively low concentrations in the heart, muscles and kidneys. Aspartate transaminase (AST) is an enzyme present in tissues of high metabolic activity and is released into the blood after cell damage. ALT and AST are both often elevated in liver disease and are an indirect measure of liver damage. These enzymes are normally inside liver cells, and their presence in the blood indicates liver cell damage.3 ALT is a better indicator of liver damage than AST, but both tests are typically ordered together. Bilirubin—the breakdown product of erythrocyte hemoglobin—is eliminated by the liver in the bile. Elevated levels can be an indication of liver damage and is seen in patients with cirrhosis and hepatitis.3 Albumin, which maintains colloidal osmotic pressure in the vascular and extravascular spaces, is a source of nutrition and part of a complex buffer system. A decrease in albumin levels can indicate an acute inflammatory infectious process. Albumin can be used to determine nutritional status, acute illness, liver and kidney damage and other chronic diseases.3
| Autoimmune Masquerader Sarcoidosis is one of the main causes of inflammatory eye disease, and one study found ocular involvement was the presenting symptom in approximately 20% to 30% of patients.2 The researchers noted uveitis, typically bilateral, granulomatous and chronic, in 30% to 70%, with conjunctival nodules seen in 40%.2 Sarcoidosis suspects require an extensive work-up, including a complete physical exam, laboratory testing (including CBC, ESR/CRP, kidney and liver assays, and angiotensin converting enzyme [ACE]) and pulmonary radiographic studies.1 Even though ACE level is elevated in 75% of untreated sarcoidosis patients, the test has limited utility due to poor sensitivity and insufficient specificity (almost a 10% rate of false positive results).1 Pulmonary radiographic studies often start with a chest radiograph, followed by high-resolution computed tomography. Bilateral hilar adenopathy is a classic finding in sarcoidosis. If the diagnosis of sarcoidosis is unclear, additional scans such as positron emission tomography or gallium-69 radioactive tracer may help.1 Case Example: The patient was diagnosed with bilateral granulomatous uveitis with elevated IOP secondary to the uveitis OD. The patient was started on Pred Forte 1% (Allergan) every hour OU, homatropine 5% BID OU and timolol 0.5% BID OD. The patient was referred to his PCP for a uveitis work-up with an emphasis on sarcoidosis testing. On follow up three days later, he showed improvement in his anterior chamber reaction (3+ OD and 2+ OS) and reported that he saw his PCP and was told there wasn’t any conclusive evidence of sarcoidosis, as his ACE testing was 48nmol/mL/min (typical adult levels between 8nmol/mL/min and 53nmol/mL/min) and they found no granulomas on his chest x-rays.3 We treated the patient over the next six months with topical steroids and oral steroids; however, whenever it appeared his inflammation had cleared and we began tapering, he would flare up. We referred the patient back to his PCP and requested repeat lab testing and advanced imaging. The patient received a gallium-69 scan, which confirmed sarcoid granulomas in his lungs. 1. Judson MA, Boan AD, Lackland DT. The clinical course of sarcoidosis: presentation, diagnosis, and treatment in a large white and black cohort in the United States. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2):119-27. |
Inflammatory Markers
Testing for systemic inflammatory markers is a crucial diagnostic component for potentially sight-threatening conditions such as ischemic optic neuropathy (ION). The two most common tests include erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).3,9
ESR. In response to acute and chronic inflammation, the amount of protein (mostly fibrinogen) increases in the plasma, encouraging the RBCs to stick together.3,4 ESR measures the rate at which the RBCs settle out of solution during a specified period of time, which can be the result of some infections, collagen-vascular diseases, inflammatory diseases and tissue damage from myocardial infarction.3 While the presence of elevated ESR is non-specific and doesn’t indicate where the inflammation is coming from, it can be used when monitoring for decreased levels. ESR is indicated in patients suspected of having temporal arteritis and uveitis-related systemic disease.3,9
CRP. This an acute phase protein that is more sensitive than the ESR, responds more quickly to the presence of inflammation and disappears faster on resolution. Standard CRP is indicated to assess a patient for systemic inflammation, while high-sensitivity CRP is primarily used for cardiac disease assessment.3,4
An ESR, CRP or both should be ordered for patients with suspected ION to help rule out the arteritic form (temporal or giant cell arteritis), especially in patients who are experiencing scalp tenderness, jaw claudication with a unilateral swollen optic nerve or both.4
| Table 5. Lab Testing for Autoimmune Disorders | |
| Autoimmune Disorder | Lab Testing |
| Rheumatoid arthritis |
|
| Systemic lupus erythematosus |
|
| Ankylosing spondylitis Psoriatic arthritis Reactive arthritis Inflammatory bowel diseases |
|
| Graves’ disease |
|
| Sarcoidosis |
|
Autoimmune Disorders
This is a varied group of conditions in which the body’s innate immune system sets up a chronic inflammatory response to its own tissues.9 Because ocular manifestations—such as dry eye, episcleritis, scleritis, uveitis, retinal hemorrhages, ION and retinal vasculitis—may be the first sign of an underlying autoimmune disease, optometrists must be aware of the possible underlying systemic cause and appropriate lab testing.9 Some of the most common autoimmune disorders that optometrists come in contact with include rheumatoid arthritis (RA), systemic lupus erythmatosus (SLE), HLA-B27-associated conditions, Sjögren’s syndrome, Graves’ disease and multiple sclerosis. Several lab tests (Table 5) can help uncover autoimmune dysfunction, including:
Rheumatoid factor (RF) and anticyclic citrullinated antibodies (anti-CCP). These two markers, used to help diagnose RA, have similar sensitivity (67% for anti-CCP vs. 69% for RF), although anti-CCP is more sensitive (95% vs. 85% for RF) in its predictive value for development of erosive disease.9,10 However, in the early stages of RA, patients may test negative with both. As there are characteristic joint changes seen in RA, patients who test negative but have symptoms should be referred for radiographic studies of hands and feet (primary tissues and joints affected in RA) for baseline and to aid in diagnosis. Other rheumatic diseases may also test positive for RF, and as patients age they may test positive for RF but not have RA.10,11
Antinuclear antibodies (ANA). The presence of ANA in serum supports an SLE diagnosis and related autoimmune diseases, while its absence in a patient with suspected SLE makes the diagnosis much less likely.12 ANA results are typically presented as an endpoint titer and the staining pattern (or patterns) produced by the patient’s serum. Nuclear staining patterns are loosely associated with the underlying autoimmune disease and include: homogeneous, speckled, centromere and nucleolar.12 ANA is primarily a screening test for lupus, but is not diagnostic of the condition, as other diseases will test positive for ANA, including scleroderma (95%), mixed connective tissue disease (100%), Sjögren’s syndrome (60%), RA (50%) and juvenile idiopathic arthritis (15% to 40%).13
Confirmatory testing is required to diagnose lupus in conjunction with presenting signs and symptoms. Antidouble-stranded DNA (anti-dsDNA) and anti-Smith (anti-Sm) antibodies are highly specific for SLE, but anti-Sm antibodies lack sensitivity. Anti-dsDNA and anti-Sm antibodies are seen in approximately 70% and 30% of patients with SLE, respectively.13 The Sjögren’s syndrome antibody Anti-Ro/SSA and anti-La/SSB antibodies are present in approximately 30% and 20% of patients with SLE, respectively; however, both antibodies are more commonly associated with Sjögren’s syndrome.11,13
Human leukocyte antigen (HLA). The HLA encodes proteins on the surface of leukocytes that have a critical role in immunity, including antigen processing and presentation to T-helper cell and self-recognition by immune cells.14 Research strongly links HLA-B27 to several spondyloarthropathies, including ankylosing spondylitis, psoriatic arthritis, reactive arthritis and the inflammatory bowel diseases (Crohn’s and ulcerative colitis).14 HLA-B27 is also strongly associated with acute anterior uveitis and recurrent acute anterior uveitis in particular, with as much as 80% of patients with recurrent acute anterior uveitis being HLA-B27.14,15 However, regardless of the strong association, research suggests HLA testing has limited usefulness in diagnostic testing in uveitis patients. Only 1% of patients who test positive for HLA-B27 are likely to develop uveitis, and patients who present with uveitis secondary to an HLA-B27 condition are likely to have other signs and symptoms indicative of the disease process.14,15 If a patient does test positive for HLA-B27, they could have one of several conditions, so it doesn’t necessarily help in the diagnostic process.
Thyroid testing. In hyperthyroidism, or Graves’ disease, an overactive thyroid gland secretes excessive T3 and T4, which results in low thyroid-stimulating hormones.16,17 Because T3 and T4 are decreased in hypothyroidism, the pituitary secretes more TSH.16,17 Ultrasensitive serum TSH studies have the highest sensitivity and specificity to screen for both hypo- and hyperthyroidism. An additional test can detect the presence of free serum T4 and T3.16
In Graves’ disease, the most common cause of hyperthyroidism, patients will experience heart palpitations, heat intolerance, weight loss, skin rash and ophthalmopathy (25% to 85%).17 The prevalence of distinct ocular abnormalities are: eyelid retraction, 92%; exophthalmos, 62%; extraocular muscle dysfunction, 43%; ocular pain, 30%; increased lacrimation, 23%; and optic neuropathy, 6%.17
Clinicians should consider TSH, free T4/T3, orbital imaging or a combination of all three in any patient exhibiting signs of Graves’ disease.16,17 Thyroid testing should also be considered for a patient presenting with superior limbic keratoconjunctivitis, which is associated with thyroid dysfunction.18 Patients typically present with a gritty or foreign body sensation, superior redness or injection and hyperemia. Slit lamp results demonstrate superior palpebral or bulbar conjunctival inflammation with the development of pannus in the superior one-third of the cornea.18
Case Example:
A 33-year-old Hispanic female presented to the clinic complaining about an acute-onset, painful red right eye. It started a couple of days ago with a “nodule” and redness, and the pain seemed to be going through her entire eye. She tried a “take the red out” eye drop that helped. Her medical history is positive for RA, diagnosed three years previously. She stated that she didn’t have a PCP at the time and had been taking Celebrex (celecoxib, Pfizer) for her joint pain. Upon further questioning, she reported she occasionally gets a rash when out in the sun for too long, and her mother also had RA.
Entering uncorrected VAs were 20/40 OD (no improvement on pinhole) and 20/20 OS. Entrance skills were unremarkable, although she did experience eye pain on eye movement. Blood pressure was 125/80mm Hg. Slit lamp exam revealed an elevated, sectoral 3+ redness on the nasal palpebral conjunctiva (the deep scleral vessels appeared to be engorged), 2+ cells and trace flare (Figure 4). OS was unremarkable. IOPs were 18mm Hg OD, OS, and dilated fundus exam revealed cotton wool spots in both eyes.
We diagnosed the patient with a non-necrotizing scleritis. Although typical first-line therapy is oral nonsteroidal anti-inflammatory drugs (NSAIDs), she was already taking Celebrex, which didn’t seem to be managing the condition.15 Upon further questioning, she was unable to tell us who diagnosed her with RA or what tests were done. With the diagnosis of scleritis and the presence of cotton wool spots in both of her eyes, we began to question her diagnosis of RA and made an urgent referral to rheumatology for SLE assessment.
The report from rheumatology confirmed a diagnosis of lupus. Her lab results were positive for ANA, and then confirmed with anti-dsDNA as well as anti-Sm. The rheumatologist was concerned she was going through a “flare up,” given her active scleritis, and additional lab testing that indicated that she had abnormal kidney, liver and cardiac enzymes. Because of these concerns, the rheumatologist bypassed the second-line therapy of oral steroids and went directly to systemic immunosuppressive therapy (oral cyclophosphamide).19 She was also taken off Celebrex and started on hydroxychloroquine 400mg per day to help manage her joint pain and skin rashes.
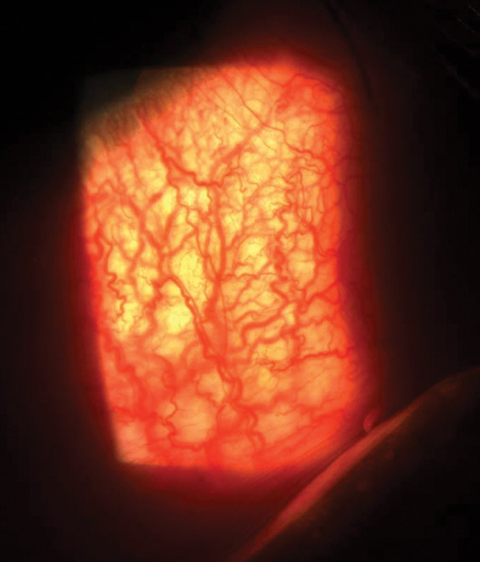 |
| Fig. 4. This 33-year-old Hispanic female presented with scleritis. This image highlights inflammation of the deeper scleral vessels. |
Infectious Disease
A variety of ocular conditions can manifest secondary to a systemic infectious disease, including hyperacute conjunctivitis, keratitis, uveitis and retinal vasculitis. The main underlying infectious diseases that can manifest ocular complications include chlamydia, gonorrhea, syphilis, herpes, tuberculosis (TB) and Lyme disease. Most of these conditions have their own diagnostic lab testing:
Nucleic acid amplification test (NAAT). This is the diagnostic test of choice for chlamydial and gonorrhea infection of the genitourinary tract and uses vaginal swabs for women or first-catch urine for men. Conjunctivitis (typically hyperacute) is the most common ocular manifestation of these conditions.1,20,21
Syphilis testing. There are two types of serologic tests for syphilis: nontreponemal and treponemal-specific. The use of only one test is insufficient for diagnosis since serologic testing (especially nontreponemal tests) can be associated with false positive results.24 Ocular syphilis can involve almost any eye structure, but posterior uveitis and panuveitis are the most common and present with diminished VA. Additional findings can include interstitial keratitis, anterior uveitis, optic neuropathy and retinal vasculitis.23
Nontreponemal tests are nonspecific and have traditionally been used for initial syphilis screening due to their relatively low cost, ease of performance and ability to be quantified for the purpose of following response to therapy.22 The tests include rapid plasma reagin (RPR), venereal disease research laboratory and the toluidine red unheated serum test.22
Treponemal tests are more complex and expensive to perform than nontreponemal tests and have traditionally been used as confirmatory tests for syphilis when the nontreponemal tests are reactive. However, newer versions of these tests are automated, enhancing simplicity and facilitating ease of use and enabling their use in initial testing.22 These test include: fluorescent treponemal antibody absorption, microhemagglutination test for antibodies to Treponema pallidum, T. pallidum particle agglutination assay, T. pallidum enzyme immunoassay and chemiluminescence immunoassay.22
Lyme testing. Lyme disease is the most common tick-borne disease in the United States, Canada and Europe.24 A variety of ocular manifestations have been associated with Lyme disease, including conjunctivitis (most common), keratitis, iridocyclitis, retinal vasculitis, choroiditis, optic neuropathy and uveitis. Serologic testing should be performed in patients who meet all of the following criteria:24
A recent history of having resided in or traveled to an area endemic for Lyme disease.
A risk factor for exposure to ticks.
Symptoms consistent with early disseminated disease or late Lyme disease (e.g., meningitis, radiculopathy, mononeuritis, cranial nerve palsy, arthritis, carditis).
Serologic testing for anti-Borrelia burgdorferi antibodies, a two-tier conditional strategy, is recommended to support the diagnosis of Lyme disease. The traditional two-tiered testing algorithm uses a sensitive enzyme immunoassay, such as a whole cell-based enzyme-linked immunosorbent assay followed by a more specific Western blot test. Separate IgM and IgG blots are typically performed.24
Tuberculosis. This disease should be suspected in patients with relevant clinical manifestations (cough of more than two to three weeks’ duration, lymphadenopathy, fevers, night sweats, weight loss) and relevant epidemiologic factors (history of prior TB infection or disease, known or possible TB exposure, past or present residence in or travel to an area where TB is endemic).25 Ocular manifestations of TB include choroiditis, chorioretinitis, choroidal granuloma, optic neuritis, orbital cellulitis, scleritis, necrotizing scleritis, posterior scleritis, interstitial keratitis and anterior chamber granuloma.26
Patients suspected of being exposed to TB should have a tuberculin skin test or interferon-gamma release assay, as they are designed for diagnosis of TB infection; a positive result supports (but cannot be used to establish) a diagnosis of active TB disease, and a negative result does not rule out active TB disease.
A chest x-ray is required, and if suspicion of TB is present, three sputum samples are recommended for smear analysis, culturing and nucleic acid amplification testing.25
Optometry plays a crucial role as part of the health care team in the management of patients’ ocular and systemic health. Optometrists must be familiar with the specific lab testing that is often required in the diagnosis and management of systemic conditions with associated ophthalmic manifestations.
Dr. Lonsberry is a professor of optometry at Pacific University College of Optometry.
1. Center for Disease Control and Prevention. Recommendations for the Laboratory-Based Detection of Chlamydia trachomatis and Neisseria gonorrhoeae—2014. MMWR 2014;63(No. RR-2). |
