 |
Scleral Lens Fitting: ONCE RARE, NOW ROUTINE?
As these specialty lenses continue to gain in popularity, should they be adopted for wear in uncomplicated cases as well?
Release Date:
April 2016
Expiration Date:
April 1, 2019
Goal Statement:
This course covers current uses for scleral lenses and discusses their potential for coverage of the normal cornea.
Faculty/Editorial Board:
 Dr. Langis Michaud, OD, graduated from École d'optométrie de l'Université de Montréal in 1986, where he also obtained his master's degree in physiological optics. He is a professor and chief of the contact lens department at the Université de Montréal, as well as a fellow of the AAO, BCLA and SCLS.
Dr. Langis Michaud, OD, graduated from École d'optométrie de l'Université de Montréal in 1986, where he also obtained his master's degree in physiological optics. He is a professor and chief of the contact lens department at the Université de Montréal, as well as a fellow of the AAO, BCLA and SCLS.
Credit Statement:
This course is COPE approved for 1 hour of CE credit. COPE ID is 48988-CL. Please check your state licensing board to see if this approval counts toward your CE requirement for relicensure.
Joint Sponsorship Statement:
This continuing education course is joint-sponsored by the Pennsylvania College of Optometry.
Disclosure Statement:
Dr. Michaud has received honororia from Valeant, CooperVision, Blanchard Labs and Allergan; is a consultant to Blanchard Labs; and has received grant/research support from Alcon, Johnson & Johnson Vision Care and Genzyme Canada. He is also on the speakers' bureau of the American Academy of Optometry and is an employee of the Université de Montréal.
Many practitioners have seen patients who benefit from scleral lens wear, such as those with irregular corneal shapes, ocular surface conditions like severe dry eye or non-healing corneal erosion, or following exposure to chemicals.1 Few adverse events have been widely linked to the use of these rigid lenses, making them arguably one of the safest options in contact lens practice. As such, most may consider them a valid possibility for patients with “regular” corneas that demonstrate some measure of refractive error but no other obvious abnormalities; however, lingering questions prevent widespread adoption.
First and foremost, there is a certain agreed-upon approach taken when fitting irregular cornea patients with sclerals—but can we use the same principles on those with normal corneas? Are these lenses safe over the long-term as a means to correct refractive error? How does their performance measure up against existing lenses for normal corneal wear? This article will offer an evidence-based approach to answer these questions.
REVIEWING THE RECORDS
The earliest published article on scleral lenses still present in the literature today dates to 1946.4 Since then, approximately 219 published works have been added, each serving to increase practitioner knowledge on scleral lens wear. Among these, six publications cover adverse events such as acute red eye, microbial keratitis and fitting complications after surgery. Microbial keratitis in particular was linked to extended and/or noncompliant wear and the presentation of severe ocular surface disease.9,24 The safety of sclerals was assessed in eight papers, none of which reported significant negative impacts from wear. Of the 219 papers, 133—including 14 retrospective studies—described the successful placement of scleral lenses on irregular corneas to improve the ocular surface.
Professional publications’ coverage also offers a way to track reports of complications related to scleral lens wear. Few articles have identified significant negative impacts, and none have been published since modern gaspermeable scleral lenses became more widely available. Based on this survey of scientific and professional literature, it can be said that scleral lenses are a relatively safe mode of contact lens wear for the clinical population who requires specialty lenses. A definitive statement on the safety of these lenses for those with normal corneas cannot be made, however, since no long-term, randomized, masked, controlled studies have been conducted on this topic.
MAKING SPACE FOR SCLERALS
Considering whether patients with normal corneas should be fit with scleral lenses to correct refractive error prompts a series of questions. First, who are candidates, and what are the clinical indications for lens wear? Additionally, which mode of lens wear should be prescribed, and how can these lenses differ from other options? Once these questions are answered, an additional one to consider is this: Can the same positive and safe outcome observed with other clinical populations be duplicated in the case of normal cornea patients? Is the risk-to-benefit ratio the same? Let’s discuss.
The clinical population in question is characterized by a prolate cornea that is—in theory—less difficult to vault than an irregular corneal surface. This is because a regular cornea is more uniform in shape, and therefore more predictable to fit. Scleral lenses placed on these corneas should correct existing refractive error, but do not need to restore the regularity of the ocular surface as they do if covering an irregular or compromised eye. However, in the absence of this traditional indication, one could argue it in essence removes the need for a scleral lens entirely and a more simple, corneal-fit lens may suffice.
In light of this, it can be argued scleral lenses are most likely to be considered for improvement of visual acuity and comfort based on two frequent issues reported by symptomatic wearers.19 Because their large diameter means a reduced lens-to-lid interaction and because they vault the most sensitive part of the human body—the cornea—without touching it, both lens awareness and mechanical stress are highly reduced in comparison with other lens options. Scleral lenses additionally do not dehydrate as soft lenses do and leave room for a fluid compartment, which contributed to the maintenance of a more properly hydrated ocular surface. This may help reduce symptoms of contact lens induced dry eye.1
Athletes and those faced with certain occupational hazards may also benefit from scleral lens wear. Once settled on the ocular surface, scleral lenses act as a shield against infiltration of dust and particles, particularly in dry and challenging environments. In some cases, this shielding aspect may also protect the eye from impact that can result in significant damage (off-label usage). The same rationale applies to patients with allergies for whom sclerals prevent encroachment of pollen and other allergens onto the ocular surface. Overall, however, the most notable feature of scleral lenses is that they do not move once fitted to the eye—a key feature for reducing higher-order aberrations or controlling more advanced astigmatism or presbyopia.
ASTIGMATISM CORRECTION
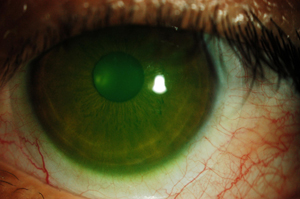 |
| A mini-scleral contact lens. Larger scleral lenses vault the cornea and land further out past the limbus. |
A simple, spherically designed scleral lens can compensate for up to 3.5D of corneal cylinder in an astigmatic patient. This exceeds the range provided by smaller, gas permeable lenses. Additionally, though most soft toric lenses include a 4.5mm to 5mm effective optic zone, this typically shrinks as toricity increases. Sclerals, in contrast, feature an 8mm to 9mm optic zone to enhance the field of vision and limit interaction with the pupil diameter and, consequently, the perception of high order aberrations. And as previously stated, scleral lenses do not rotate or dehydrate, keeping the patient’s quality of vision optimal for the entire period of time they’re worn.
Once the lens is placed on the eye, it’s common to assess the amount of residual astigmatism. One source for such findings is the presence of lenticular astigmatism. Patients with this type of astigmatism inherently compensate, in whole or in part, for corneal cylindrical power; fitting them with a scleral lens, however, leads to the fluid layer compensating instead for the toric corneal surface, thus revealing the lenticular astigmatism. The addition of a front-toric design to the scleral lenses can help adjust the visual correction for such a patient.
Residual astigmatism can also come from lens flexure.2 This may be a misleading concept to some: the supposed flexure of the lens is a process that is assessed using keratometry or topography over the scleral lens while the eye is open. Flexure cannot happen, however, if the eye does not blink; as such, what is actually measured here using overkeratometry is lens distortion originating primarily from the misalignment of the lens peripheries on the toric conjunctival surface. When this occurs, increasing the lens’s thickness—a commonly relied-upon solution— is actually detrimental, as it can penalize oxygen delivery to the cornea and make the lens heavier and easier to decenter. Instead, resolve the issue using a lens with toric haptics to achieve a better lens/conjunctival alignment in all quadrants. To the contrary, better aligned lenses can certainly be manufactured thinner, which is healthier for the cornea over the long term.
If the scleral lens does decenter or is placed in the presence of a highly irregular cornea, however, the fluid layer between it and the contact lens can lose its symmetrical shape and become prismatic. This is the primary cause of in-duced residual astigmatism.17 This decentration can also increase lens bearing on the superior quadrant of the cornea; as such, it can be resolved by reducing the lens’s diameter or adding toric peripheral curves to improve centration.
If neither of these solutions can be applied, directing the laboratory to increase the optic zone diameter while keeping the sag value the same is another option. Keep in mind when doing this, however, that other parameters will change accordingly. Of course, whatever method you as a practitioner use, the end goal should remain the same: to increase uniformity of the tear fluid layer and keep the lens centered on the surface of the eye. At last, front-toric designs will resolve this issue.
PRESBYOPIA CORRECTION
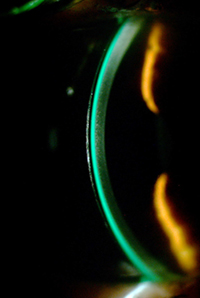 |
| Mini-scleral lenses can be fit with less tear fluid to optimize oxygen delivery to the cornea. |
Patients entering the presbyopia category this decade number more than ever before, which is why many lens manufacturers are developing new designs to meet their visual needs.3 Several soft lens modalities have been launched in the last few years, most notably in the daily disposable lens market. Despite these new offerings, however, contact lens dropout remains remarkably high in the presbyopic population. This is attributed to the somewhat unstable tear film most aging patients exhibit in comparison with their younger counterparts, and can thus be considered to have marginal dry eye. Many presbyopic patients also display significant refractive astigmatism that, if not adequately corrected by optic means, can lead to fluctuating and distorted visual acuity at distance and up close. Unfortunately, few new toric multifocal contact lenses to date offer a positive outcome for presbyopes with astigmatism, especially in disposable modalities.
Scleral contact lenses, however, may be an option. The fluid layer underneath the lens keeps the ocular surface moist and hydrated, stabilizing the tear film. Furthermore, these lenses compensate for some amount of refractive astigmatism; additionally, the larger optic zone present in the traditional scleral lens design also means room for larger add power zones with unaffected distance vision. These elements mean lens designers have an easier time manufacturing functional multifocal contact lenses. Furthermore, sclerals—especially smaller, minisclerals that measure less than 15mm in diameter—remain better aligned with a patient’s visual axis.16
FITTING THE NORMAL CORNEA
Successful adaptation of scleral lenses for patients with normal corneas requires more than just the recognition of their optical benefits for current wearers, however. For this broad population to accept sclerals as a modality, the lenses must be made easier to care for and more convenient to wear. Improper lens handling still represents the biggest concern for current wearers and is one of the primary reasons for fitting failures. Unsurprisingly, smaller scleral lenses (i.e., 15mm or less) are better for prolate patients as the size of these lenses is similar to that of soft torics. Sclerals of a larger diameter (i.e., 16.5mm to 17mm) may be more intimidating and less user-friendly compared with their miniature counterparts. The same rationale applies for lens care; use of hydrogen peroxide is one method to improve wear and care compliance.
Are scleral lenses a safe alternative to soft lens modalities, then? Currently, there are no longitudinal studies establishing the safety of scleral lens wear for normal cornea patients. As such, questions remain unanswered in this area, which is why the risk-to-benefit ratio remains under debate at this time. Scleral lenses and the fluid layer under their surface act as a reservoir to keep the ocular surface moist, and it has been demonstrated that the ideal combination of lens and fluid layer thicknesses are 250μm and 200μm, respectively, in compliance with the Harvitt-Bonnano criteria for alleviating corneal hypoxia.13 Lenses fitted with higher clearance and/or produced with increased thickness are known to be associated with central corneal edema sustained during all wearing hours. Of course, this model has been challenged clinically since its conception because many practitioners have reported no obvious signs that chronic corneal hypoxia had occurred. Additionally, almost no reports of corneal hazing or the presence of microcysts or neovascularization have been collected, and it has also been argued that since scleral lenses have been successfully used to treat ocular surface disease, it would be impossible for hypoxia to be involved.
Clinical studies have since been published confirming that scleral lens wear is associated with induced corneal swelling varying from 2% to 4% in normal corneas, keratoconus and—especially—in cases where the endothelial cell layer is compromised.6,12,14,15,18,20 One in vivo study also indicated reduced oxygen diffusion to the cornea correlates with less tear fluid layer thickness.10 In fact, large scleral lenses with a 400μm fluid layer thickness delivered 30% less oxygen to the cornea than a similarly sized lens fitted with a 200μm fluid layer thickness.10 From other studies, we also know that tear exchange is limited once the lens settles at 0.2% per minute.22 This means it takes more than eight hours to replenish the bowl under a scleral lens.
Tear mixing is another factor that should be accounted for, as the tear layer is a dynamic, constantly changing fluid environment. Like water in a washing machine, it was suggested that the deeper layer of fluid periodically makes contact with the underside of the scleral lens to replenish its oxygen levels. To the contrary, data has suggested that that tear mixing may be limited in the case of lenses fitted with more or less than the optimal level of clearance, which has been established as 200μm.23 Tear exchange may also be inhibited when clearance is particularly excessive. Consequently, the addition of fresh tears and tear mixing may only marginally assist with maintaining the cornea’s oxygen supply once the lens settles; as such, this may be a decisive factor in determining whether patients with otherwise healthy, normal corneas should wear scleral lenses.
REMODELING
Considering these factors, it can be argued that the theoretical model for oxygen diffusion should change as follows: Increased lens thickness (i.e., more than 250μm) and increased fluid layer thickness or clearance (i.e., more than 200μm) triggers corneal hypoxia. This affects the central cornea because the clearance over the limbus never exceeds the critical threshold mentioned above. This hypoxia can be transient in nature if fluid loss in the first hours reduces clearance to below the critical threshold of 200μm. As such, this is why hypoxia is not always clinically visible.
Corneal edema manifests when hypoxia reaches 5% to 8%, with clinical signs of the condition correlating with the amount of swelling.8 Loss of corneal transparency occurs when the edema reaches 15%.7 Neovascularization occurs when hypoxia turns chronic and begins to affect the limbus. Blebs are transient and not easily discernible, except in the minutes following awakening.24 Additionally, epithelial microcysts are associated with overnight wear of less oxygen-permeable soft lenses. Hypoxia has never been reported in patients who only wear lenses during the day only, even if these lenses’ oxygen permeability was below the Holden-Mertz criteria.11 Overnight wear of scleral lenses is not recommended, as it is connected with high levels of corneal hypoxia and the potential for microbial keratitis.25
CLINICAL IMPLICATIONS
Many clinical studies on pachymetry have proven that hypoxia occurs. More convincingly, however, equivalent oxygen percentage (EOP) is reduced when the clearance under scleral lenses is higher. Some authors consider 3% edema to be clinically insignificant comparable to the physiological edema seen upon awakening. They also consider this level to be similar to that encountered when patients were fit with low oxygen-permeable hydrogel lenses in the 1980s. These comparisons are misleading, however. Physiological edema never lasts for more than an hour and, as such, the cornea is never exposed to chronic hypoxic stress during waking hours. As for the aforementioned hydrogel lenses, at that time in history no other soft lens options were available. This pushed the industry to develop higher oxygen-permeable materials.
Epithelial bogging, tear reservoir debris accumulation, conjunctival prolapse and the need to design complicated toric peripheral curves or haptics are just a few of the day-to-day challenges that those who fit scleral lenses face when using larger-diameter lenses.5 These occurrences are considered benign at present. Again, there is no longitudinal study proving the presence or absence of negative impacts from these elements on ocular health or surface structure over time. Additionally, these complications are typically unseen when scleral lenses are fitted with a diameter of 15mm or less, as of this size tend to generate less mechanical impact on the conjunctiva and are fitted with lower clearance over the limbus. It can be said this represents an important element in reducing the pollution of the tear fluid reservoir with lipids and mucin deposits seen when scleral lenses impact the conjunctival cells more significantly.
In summary, there are many clinical indications to consider when fitting scleral lenses on patients with ‘normal’ corneas. Though the benefits of these lenses are numerous, practitioners must first evaluate the risk/benefit ratio of wear. In particular, long-term safety should be explored. Additionally, the lower rate of complications associated with smaller sclerals may also influence the practitioner’s selection. Lastly, in order to consider fitting normal cornea patients with scleral lenses, an easier and more convenient approach to the fitting process much be developed. For all of these reasons, mini-scleral lenses, with their limited thickness and clearance, may be the best and safest alternative at present; however, further research and consideration is necessary.
References
- Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012 Dec;35(6):272-6.
- Barnett, M. 10 Tips for Smarter Scleral Lens Fitting. Review of Cornea and Contact Lenses. Oct. 2012.
- Barnett M. Multifocal scleral lenses. Contact Lens Spectrum, Dec. 2015.
- Carlson JJ, Silbert M. The technique of fitting scleraform contact lenses; determination of the shape of the human eye by insertion of spherical contact lenses. Opt J Rev Optom. 1946 Oct;83(20):34-6.
- Caroline P. Managing corneal-scleral lenses and scleral lenses complications. Global Specialty Lens Symposium, 2014.
- Compañ V, Oliveira C, Aguilella-Arzo M, et al. Ox-ygen diffusion and edema with modern scleral rigid gas permeable contact lenses. Invest Ophthalmol Vis Sci. 2014;55:6421–6429.
- Efron N. Contact lens-induced changes in the anterior eye as observed in vivo with the confocal microscope. Prog Retin Eye Res. 2007 Jul;26(4):398-436.
- Efron N, Ed. Stromal edema. Contact Lens Com-plications. 2nd ed. Edinburgh: Butterworth-Heine-mann, 2004:132–140.
- Fernandes M. Sharma S. Polymicrobial and microsporidial keratitis in a patient using Boston scleral contact lens for Sjogren’s syndrome and ocular cicatricial pemphigoid. Cont Lens Ant Eye. 2013 Apr;36(2):95-7.
- Giasson C.J. Morency J. Michaud L. Measuring oxygen levels under scleral lenses of different clearances. Investigative Ophthalmology & Visual Science. June 2015;56:6074.
- Holden BA1, Sweeney DF. The significance of the microcyst response: a review. Optom Vis Sci. 1991 Sep;68(9):703-7.
- Lau J. Reeder R. Localized corneal graft rejection from scleral lens wear with excessive limbal clearance. Poster presented at the GSLS meeting, Las Vegas, 2015.
- Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012 Dec;35(6):266-71.
- Miller WL Vance K. Johnson L, Bergmanson JP. Scleral contact lens effect on central and peripheral corneal thickness. Investigative Ophthalmology & Visual Science. June 2015;56:6103.
- NG LH, Wang Z, Chan CY, Yueng WN. Corneal physiological changes after short-term scleral lens wear. Paper presented at BCLA meeting, Liverpool, UK, 2015.
- Plainis S, Atchison DA, Charman WN. Power profiles of multifocal contact lenses and their interpretation. Optom Vis Sci. 2013 Oct;90(10):1066-77.
- Ramdass S, Rosen C, Norman C, Buckingham R. Clinical analysis of scleral lenses on normal corneas. Poster presented at Global Specialty Lens Sympo-sium, 2016.
- RiffB. Lasby A. Pack L. Corneal decompensation after scleral lens wear in a compromised cornea. Poster presented at the GSLS meeting, Las Vegas, 2015.
- Rumpakis J. New data on contact lens dropouts: An international perspective. Rev Optom. 2010 Jan;147(1):37-42.
- Soeters N, Visser ES, Imhof SM, Tahzib NG. Scleral lens influence on corneal curvature and pachymetry in keratoconus patients. Cont Lens Anterior Eye. 2015 Aug;38(4):294-7.
- Van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral contact lenses: A review. Cont Lens Anterior Eye. 2014 Aug;37(4):240-50.
- Vance KD. Miller W. Bermangson J. Measurement of tear flow in scleral contact lens wearers. Poster presented at the American Academy of Optometry meeting, 2015.
- Yuan T, Tan B, May A, et al. Lin M. Peripheral tear mixing under scleral lenses fitted with various clearances. Paper presented at the AAO Meeting, 2015.
- Holden BA, Williams L, Zantos SG. The etiology of transient endothelial changes in the human cornea. Invest Ophthalmol Vis Sci. 1985 Oct;26(10):1354-9.
- Zimmerman AB. Marks A. Microbial keratitis secondary to unintended poor compliance with scleral gaspermeable contact lenses. Eye Contact Lens 2014, Jan;40(1):e1-4.
