A Comprehensive Look at Dry Eye Therapy
With such a robust dry eye toolbox, knowing the best approach can be tricky. This run-down of options will help clarify the treatment strategies at your disposal.
By Justin Kwan, OD
Release Date: May 2017
Expiration Date: May 15, 2020
Goal Statement: Because dry eye is a multifaceted diagnosis, optometrists need to stay current with rapid advances that change current treatments and how optometrists manage dry eye patients. This article discusses the keys to diagnosing dry eye and the myriad treatment options available to help patients manage their specific form of dry eye, whether it’s meibomian gland dysfunction, aqueous deficient dry eye or caused by an outside irritant such as cosmetics or Demodex.
Faculty/Editorial Board: Justin Kwan, OD
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 53476-AS. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Joint-Sponsorship Statement: This continuing education course is joint-sponsored by the Pennsylvania College of Optometry.
Disclosure Statement:
Authors: Dr. Kwan has no relationships to disclose.
Peer Reviewers: One reviewer is a consultant for Shire Pharmaceuticals and Santen Pharmaceuticals.
Editorial staff: Jack Persico, Rebecca Hepp, William Kekevian, Michael Riviello and Michael Iannucci all have no relationships to disclose.
As a multifaceted disease, dry eye demands an equally diverse treatment approach with every patient. Clinicians have myriad treatment avenues to explore until they find the best solution—even for those who present with two or more conditions at play. New diagnostic technology complements new treatment modalities, creating the opportunity to not only diagnose the condition better, but also treat it more effectively than ever before. Let’s take a comprehensive look at the latest tools and treatments that have revolutionized dry eye management—and the mainstays that still play a crucial role.
Diagnosis is Key
The best way to start treating, even if it’s first-line therapy, is to identify those patients who don’t even know they have a problem. Revamping the health history form and including the SPEED or OSDI questionnaire can be the best time spent by the patient and becomes an educational tool. Patients may be surprised to find that their symptom scores land them in a moderate or severe classification. The case history then becomes more focused, and clinicians can dig deeper to understand the underlying cause of the patient’s symptoms.
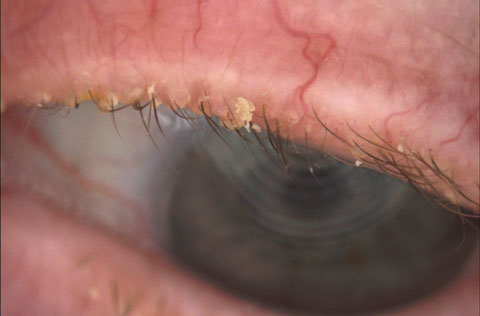
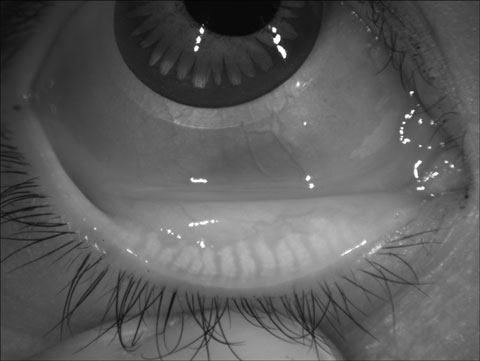
Demodex is also a common cause of dry eye symptoms, and classic signs include cylindrical dandruff and distention of the eyelash base (Figure 1). End-stage Demodex presents as chronically inflamed eyelids, madarosis and severe itchiness (Figure 2).
 |
| Fig. 1. Pervasive cylindrical dandruff and thinning eyelashes are signs of a Demodex infestation. Click image to enlarge. |
 |
| Fig. 2. This patient has end-stage Demodex with madarosis. Click image to enlarge. |
Because symptoms of Demodex, allergic conjunctivitis, MGD and ADDE often overlap, these four conditions should always be at the forefront when a patient presents with a complaint of dry eye.
Another important factor in dry eye that is recently gaining attention is cosmetics and makeup removal. The environmental working group surveyed 2,300 people and found that the average woman uses 12 products around, and inadvertently in, their eyes.5 For example, some patients apply eyeliner not only to the outer lash line but also the inner water line, directly over the meibomian gland orifices. Cosmetics are largely unregulated, and offending agents such as parabens and isopropyl cloprostenate promote inflammation and dry eye.6 Questioning a patient’s cosmetic use can often help clinicians better diagnose even the simplest cause behind dry eye.
Dry Eye Imaging
Educating patients with pictures of their own eyelids, meibomian glands, tear meniscus height and ocular surface staining often helps them better understand the underlying mechanisms of their specific form of dry eye—not to mention providing incentive to be more compliant with treatment. With meibography, both patients and doctors can view the structural integrity of the meibomian glands, which is especially helpful for patients with MGD (Figure 3). However, the degree of atrophy doesn’t consistently correlate with symptoms, tear break-up time (TBUT) or Schirmer.7
Structure is one thing, but function is another, and imaging can only go so far in guiding treatment. Ultimately, clinical acumen will help uncover the specific needs of the patient. For example, sometimes all the glands will appear intact, but gentle fingertip expression will yield nothing. Regardless of the imaging, this patient would benefit from a targeted management strategy to clear the glands.
Tried-and-True Treatments
For most patients with DED, the first treatment is artificial tears—and at the end of the day, we know many patients self-prescribe. Practitioners must be familiar with the eye drop aisle—90% of which serves ADDE, not MGD. Clinicians should recommend patients use preservative-free formulations whenever possible, considering preservatives such as benzalkonium chloride (BAK) are cytotoxic to ocular surface epithelia.
Emulsions with liquid lipids, which may better stabilize and support the lipid layer of the tear film, can be either charged or uncharged microemulsions and liposomes. Charged microemulsions, such as Retaine MGD (carboxymethylcellulose sodium 0.5%, Ocusoft) and Systane Balance (propylene glycol 0.6% ophthalmic solution, Alcon), show improvements in symptoms and corneal staining when compared with aqueous eye drops.8,9 Uncharged microemulsions such as Refresh Optive Advanced (carboxymethylcellulose sodium 0.5%, glycerin 1.0%, polysorbate 80 0.5%, Allergan) may also improve a patient’s symptoms, OSDI score and TBUT.10
But artificial tears simply won’t cut it for MGD or any number of other DED manifestations. Warm compresses and lid hygiene continue to be the main two treatments when MGD and blepharitis are the cause of the dry eye symptoms. The ideal temperature must be at least 40°C for the heat to reach the meibomian glands.11 Clinicians can prescribe a warm compress—such as a Bruder mask, ThermoEyes (Ocusoft), TheraPearls (Bausch + Lomb) or TranquilEyes (Eye Eco)— that can be microwaved for 10 to 25 seconds and sustain dry or moist heat for more than five minutes. Because the goal is to melt viscous or hardened meibum, the ideal time to use a warm compress is morning and mid-day, as most patients wake up with their eyes feeling very dry due to the lack of blinking during sleep.
 |
| Fig. 3. Meibography shows more than 50% meibomian gland atrophy of the lower lid. Click image to enlarge. |
Lid hygiene is particularly important for patients with dry eye stemming from an overgrowth of eyelid and eyelash bacteria and build up of cosmetics. With cosmetics, the first step to treatment is often education on proper and daily removal. Baby shampoo can be a cost-effective option to clean the lid margin, although all-natural alternatives such as jojoba, coconut or olive oil would be ideal for general and waterproof makeup removal, as they contain antibacterial and anti-inflammatory properties that can soothe irritated skin.12 Commercially available lid scrub wipes and foam cleansers are another option for makeup removal and lid hygiene in general.
When treating Demodex, using lid scrubs with tea tree oil is the common approach, as it provides anti-inflammatory, antimicrobial and antifungal properties.13-15 Mild cases can be treated at-home with Cliradex (Bio-Tissue), SteriLid (TheraTears), Blephadex (Lunovus) or Ocusoft scrubs BID. More stubborn cases of Demodex may warrant a higher concentration solution for use in-office.
Hypochlorous acid—such as Avenova with Neutrox 0.01% HOCL (NovaBay) or over-the-counter Hypochlor gel 0.02% HOCL (Ocusoft)—is another treatment option, as it can normalize the eyelid and eyelash environment without a laundry list of ingredients.16
In-office Tools
In-office procedures also help differentiate your dry eye management. Lipiflow (TearScience) heats the meibomian glands from the inside out and evacuates the meibum with an air bladder, while the MiBoFlo (Mibo Medical Group) heats the glands from the outside in. For practices without these treatment units, two simple handheld instruments—golf club spud and Mastrota paddle (Ocusoft)—can really make a difference. Research shows the technique of eyelid margin debridement scaling, when done on the lower eyelid margin, improves the number of meibomian glands yielding liquid secretion and improves symptoms per the SPEED questionnaire.17 The process of debriding the material, nasal to temporal, of each lower eyelid using the golf club spud takes less than 10 seconds per eye and doesn’t require anesthetic. After the procedure, clinicians can use the Mastrota paddle for a therapeutic expression and evacuation of the stagnated meibum. These two procedures work in tandem, as debridement opens up some of keratinized epithelium, making the gland expression that much more effective. The BlephEx (Rysurg) device can also help clinicians perform eyelid margin debridement while also cleaning the eyelashes.
The occasional capped gland may appear on lower or upper eyelids. Using a cotton-tipped applicator moistened with contact lens multipurpose solution, clinicians can gently scrub until the cap is removed. However, spotting the orifice metaplasia even before the capped glands form is critical, as these are more easily expressed (Figure 4).
The goal of in-office treatments is to do for the patient what they cannot consistently or effectively do themselves, which is valuable to keep them on the path of relief.
 |
| Fig. 4. Orifice metaplasia and irregularity in the eyelid margin, as seen here, are key indicators of the underlying meibomian gland structure and function. Click image to enlarge. |
Contact Lenses
For some, contact lenses can help alleviate symptoms associated with dry eye.18-20 Research shows patients with dry eye can find improved comfort after switching to a daily disposable, or from hydrogel to silicone hydrogel lenses.18-20 Also, a premium daily disposable soft contact lens may protect a patient’s sensitive cornea and help them overcome extreme light sensitivity that may make it difficult for them to keep their eyes open both indoors and outdoors. This approach is most often used for post-refractive surgery cases such as PRK, LASEK and corneal collagen crosslinking.21
Scleral lenses are also a viable treatment option for severe dry eye.22 They create a tear reservoir that lubricates the corneal surface while maintaining the oxygen supply, not to mention they can mask surface irregularities that may contribute to visual issues.
Amniotic Membranes
Research shows using an amniotic membrane for treating persistent corneal epithelial defects due to severe dry eye can hydrate and oxygenate the corneal tissue, promote epithelial healing and reduce inflammation.23 However, although an amniotic membrane makes sense to accelerate healing, repeated use for recalcitrant cases is not a long-term solution secondary to cost and inconvenience.
Oral Meds
Oral antibiotics such as minocycline, doxycycline and azithromycin can work to reduce inflammation and growth of lid bacteria by various mechanisms, one of which is to decrease MMP-9 expression, a known biomarker produced by inflamed epithelial cells.24 Because azithromycin’s stimulatory effects are unique and not the same as the tetracycline family, a patient can respond to one and not the other if there are no contraindications.25
These oral medications should only be reached for once a year to minimize bacterial resistance. From there, Restasis (cyclosporine, Allergan) or Xiidra (lifitegrast, Shire), along with triglyceride omega-3 fish oils, can build on the groundwork done by the oral antibiotics. These can be started concurrently for the severely symptomatic patient.
One study that looked at the use of re-esterified omega-3 fish oil at baseline, six weeks and 12 weeks found many dry eye parameters improved by six weeks.26 However, a clinically significant improvement in symptoms didn’t occur until the 12-week mark.26 The delayed effect could be due to the time it takes for the eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) to saturate in the red blood cells and then reach the meibomian glands. After starting patients on any therapy that takes time to ramp up, clinicians should schedule the first follow up two months from the initial visit. In addition, new research suggests oral supplementation with omega-3 and -6 stimulates the accumulation of small neutral lipid-containing vesicles in the meibomian glands.27
Topical Options
When it comes to topical prescription options for DED, most clinicians start with Restasis. Research shows cyclosporine reduces inflammation by inhibiting T-cell activation and downregulating inflammatory cytokines in the conjunctiva and lacrimal gland, thus enhancing tear production.27,28 Xiidra is a new class of drugs known as lymphocyte function-associated antigen-1 (LFA-1) antagonists, which inhibits T-cell recruitment and activation associated with DED inflammation.29,30 Clinical trials showed participants using Xiidra had a statistically significant clinical improvement in corneal staining and eye dryness compared with placebo.31
But for some patients, more than one topical treatment is necessary. In these cases, topical nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids may help.
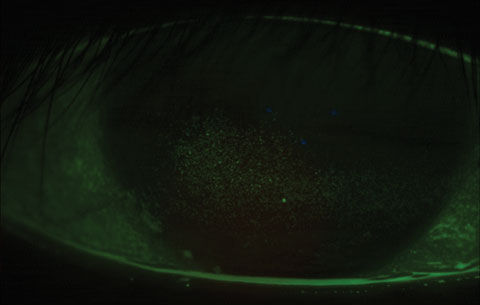 |
| Fig. 5. Coalesced corneal staining is common with post-LASIK dry eye in the first one to four weeks postoperatively. Click image to enlarge. |
NSAIDs inhibit different forms of the cyclooxygenase enzyme, thus reducing prostaglandin production and treating inflammation.32 While useful in the short-term, clinicians should use NSAIDs cautiously, as they have been known to reduce corneal sensitivity, increasing the risk of additional insult to the epithelium.33 BromSite (Sun Ophthalmics) was recently approved to treat pain after cataract surgery. It contains the NSAID bromfenac 0.075% and has the DuraSite vehicle that turns into a gel to coat the ocular surface and increase retention time and delivery of the drug to target tissues. NSAIDs for pulse treatment of dry eye is off label but can really help dry eye patients who experience ocular pain in the short term.
Corticosteroids, such as Lotemax (loteprednol etabonate, Bausch + Lomb), are more potent than NSAIDs and reduce ocular inflammation.34 For one, research suggests topical administration of methylprednisolone 1% ophthalmic solution for several weeks provides moderate, or even complete, relief of dry eye symptoms.35 Clinicians should monitor patients treated with topical corticosteroids closely for known risks such as cataract formation, glaucoma, corneal thinning and infectious keratitis.36 Lotemax gel in particular provides a consistent concentration of 0.5% loteprednol etabonate without having to shake the bottle.
Autologous serum, as a dry eye treatment and for ocular surface healing, is the most natural, compatible component that can be added to the eye since it’s derived from blood plasma. It contains anti-inflammatory factors that ultimately inhibit the ocular surface inflammatory cascade responsible for dry eye.37 While some studies show autologous serum drops improve ocular irritation symptoms, a recent Cochrane Review did not find conclusive evidence of its benefits compared with artificial tears.38-40
Punctal Plugs
For patients with ADDE, punctal plugs work wonderfully. Patients should be prepared for delayed gratification, however, as research shows patients did not see a dramatic improvement in symptoms, Schirmer’s and tear break-up time until six months post-insertion of permanent punctal plugs.41
Many patients have post-LASIK dry eye, and micro and macro punctate staining is often seen in the first one to four weeks postoperatively (Figure 5). Ninety or 180-day dissolvable collagen punctal plugs work well during this time to hold more aqueous tears on the ocular surface while the corneal nerves regrow and the lacrimal gland is signaled to produce aqueous at a normal level again. Post-LASIK patients are also dumping significant amounts of BAK onto the ocular surface with the prophylactic antibiotic eye drops and corticosteroid eye drops that first week, possibly adding to the epithelial irritation.
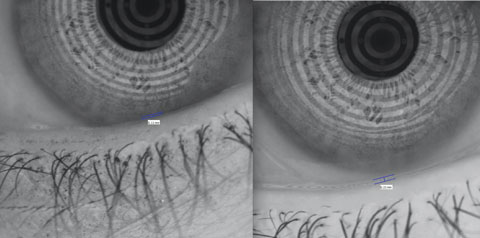 |
| Fig. 6. Punctal plugs can double the tear meniscus height, as seen here. Click image to enlarge. |
Many contact lens wearers struggle with dry eye, and punctal plugs can help. In one case, permanent punctal plugs helped elevate the tear meniscus height of a 49-year-old female by almost double, even while wearing a soft contact lens during both measurements (Figure 6). The first sign of dryness can be intermittent or constant blurry vision, mainly because the prelens tear film is thin and breaks down easily.42 Research shows a lipid-based artificial tear can be a beneficial rewetting drop to extend comfortable contact lens wearing time and reduce lid wiper epitheliopathy, as well as corneal staining.43
Prescribe a Lifestyle Change
Getting to know the patient’s work environment and how they view their computer monitor(s) can be a key component to dry eye therapy. Too many computer users continue to look straight or upwards at their monitors on stands. The preferred slight down gaze reduces the palpebral aperture size and keeps the tear film more stable.44 It also reduces the muscle strain caused by keeping the upper eyelid in a higher position than necessary. Encouraging patients to raise their chairs, lower their monitors and blink more often are simple first steps to minimizing dry eye related to close computer work.
Research shows digital device use affects blink rate and completeness, thereby affecting tear film stability.45,46 A free computer application called EyeLeo encourages blinking and other short, seven-second exercises every 10 to 15 minutes and suggests a longer break once an hour. While the frequency may seem excessive, the patient can begin to understand that blinking ensures the flow of meibum and keeps the eyes from becoming excessively strained or tired. In addition, an occupational computer lens specific to the workstation set up and accommodative demand would be a necessary tandem prescription.
Dry eye therapies, on their own, can be simple in mild cases; however, once patients begin to use more than a few all-natural treatments and still don’t find relief, short courses of prescription medications are necessary. Knowing mechanisms of action and anticipating the time it takes to feel an effect are essential to proper management. Working with a team approach with other optometrists and ophthalmologists, particularly when scleral lenses are indicated, can greatly improve a dry eye patient’s quality of life.
The overall goal of dry eye therapy is to be preventative and promote long-term wellness, not just prescribe a palliative artificial tear. Too many interventions at once could affect the patient’s compliance and may mask what is, and is not, working. Luckily, clinicians see dry eye patients regularly, providing an opportunity to build a long-lasting relationship. If we can meet patients where they are and understand their struggles, we provide compassionate care that’s highly customized. In the end, it’s rewarding for both patients and practitioners alike.
Dr. Kwan is an assistant professor at Southern California College of Optometry at Marshall B. Ketchum University. He is the current chief of the Stein Family Cornea and Contact Lens Center, University Eye Center, Ketchum Health. He is also director of the Dry Eye Institute for patient care and participates in dry eye and contact lens research.
|
1. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-8. 2. Nichols K, Foulks G, Bron A, et al. The International Workshop on Meibomian Gland Dysfunction: Executive Summary. Invest Ophthalmol Vis Sci. 2011;52(4):1922–9. 3. Nelson JD, Shimazaki J, Benitez-del-Castillo JM, et al. The international workshop on Meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2011;52(4):1930-7. 4. Blackie CA, Korb DR, Knop E, et al. Nonobvious obstructive meibomian gland dysfunction. Cornea. 2010 Dec;29(12):1333-45. 5. Environmental Working Group. Exposures add up – survey results. www.ewg.org/skindeep/2004/06/15/exposures-add-up-survey-results. Accessed March 15, 2017. 6. Food and Drug Administration. Warning letter. www.fda.gov/ICECI/EnforcementActions/WarningLetters/ucm251951.htm?sms_ss=email&at_xt=4db10c8089a4ed56%2C0. April 18, 2011. Accessed March 15, 2017. 7. Machalinska A, Zakrzewska A, Safranow K, et al. Risk factors and symptoms of meibomian gland loss in a healthy population. J Ophthalmol. 2016;2016;7526120. 8. Amrane M, Creuzot-Garcher C, Robert P-Y, et al. Ocular tolerability and efficacy of a cationic emulsion in patients with mild to moderate dry eye disease–A randomised comparative study. J Fr Ophthalmol. 2014;37(8):589-98. 9. Aguilar AJ, Marquez MI, Albera PA, et al. Effects of systane Balance on noninvasive tear film break-up time in patients with lipid-deficient dry eye. Clin Ophthalmol. 2014;8:2365. 10. Simmons PA, Carlisle-Wilcox C, Chen R, et al. Efficacy, safety, and acceptability of a lipid-based artificial tear formulation: a randomized, controlled, multicenter clinical trial. Clinical Therapeutics. 2015;37(4):858-68. 11. Bron AJ et al. Functional aspects of the tear film lipid layer. Exp Eye Res. 2004 Mar;78(3):347-60. 12. Pazyar N, Yaghoobi R, Ghassemi MR, et al. Jojoba in dermatology: a succinct review. G Ital Dermatol Venereol. 2013;148(6):687-91. 13. Cox S, Mann C, Markham J. Interactions between components of the essential oil of Melaleuca alternifolia. J Appl Microbiol. 2001;91(3):492-7. 14. Hart P, Brand C, Carson C, et al. Terpinen-4-ol, the main component of the essential oil of Melaleuca alternifolia (tea tree oil), suppresses inflammatory mediator production by activated human monocytes. Inflamm Res. 2000;49(11):619-26. 15. Thomsen N, Hammer K, Riley T, et al. Effect of habituation to tea tree (Melaleuca alternifolia) oil on the subsequent susceptibility of Staphylococcus spp. to antimicrobials triclosan, tea tree oil, terpinen-4-ol and carvacrol. Int J Antimicrob Agents. 2013;41(4):343-51. 16. Debabov D, Noorbakhsh C, Wang L, et al. Avenova with Neutrox (pure 0.01% HOCl) compared with OTC product (0.02% HOCl). NovaBay Pharmaceuticals, Inc. http://novabay.com/wp-content/uploads/2015/05/avenova-with-neutrox-first-and-only-product-in-ophthalmology-containing-pure-hypochlorous-acid-compared-with-otc-product.pdf. Accessed: September 14, 2016. 17. Korb DR, Blackie CA. Debridement-scaling: a new procedure that increases meibomian gland function and reduces dry eye symptoms. Cornea. 2013;32(12):1554-7. 18. Chalmers R, Long B, Dillehay S, Begley C. Improving contact lens related dryness symptoms with silicone hydrogel lenses. Optom Vis Sci. 2008;85(8):778–84. 19. Chalmers R, Dillehay S, Long B, et al. Impact of previous extended and daily wear schedules on signs and symptoms with high Dk lotrafilcon A lenses. Optom Vis Sci. 2005;82(6):549-54. 20. Schafer J, Mitchell GL, Chalmers RL, et al. The stability of dryness symptoms after refitting with silicone hydrogel contact lenses over 3 years. Eye Contact Lens. 2007;33(5):247-52. 21. Xie WJ, Zeng J, Cui Y, et al. Comparison of effectiveness of silicone hydrogel contact lens and hydrogel contact lens in patients after LASEK. Int J Ophthalmol. 2015;8(6):1131-5. 22. Yuksel E, Bilgihan K, Novruzlu S, et al. The management of refractory dry eye with semi-scleral contact lens. Eye Contact Lens. May 19, 2016. [Epub]. 23. Tosi GM, Massaro-Giordano M, Caporossi A, et al. Amniotic membrane transplantation in ocular surface disorders. J Cell Physiol. 2005;202(3):849-51. 24. Xiao Q, Tan Y, Lin Z, et al. Minocycline inhibits inflammation and squamous metaplasia of conjunctival tissue culture in airlift conditions. Cornea. 2016;35(2):249-56. 25. Liu Y, Kam WR, Ding J, Sullivan DA. Can tetracycline antibiotics duplicate the ability of azithromycin to stimulate human meibomian gland epithelial cell differentiation? Cornea. 2015;34(3):342-6. 26. Epitropoulos AT, Donnenfeld ED, Shah ZA, et al. Effect of oral re-esterified omega-3 nutritional supplementation on dry eyes. Cornea. 2016;35(9):1185-91. 27. Liu Y, Kam WR, Sullivan DA. Influence of omega 3 and 6 fatty acids on human meibomian gland epithelial cells. Cornea. 2016;35(8):1122-6. 28. Sall K, Stevenson OD, Mundorf TK, et al. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. Ophthalmology. 2000;107(4):631-9. 29. Stevenson D, Tauber J, Reis BL, et al. Efficacy and safety of cyclosporin A ophthalmic emulsion in the treatment of moderate-to-severe dry eye disease: a dose-ranging, randomized trial. Ophthalmology. 2000;107(5):967-74. 30. Sun Y, Zhang R, Gadek TR, et al. Corneal inflammation is inhibited by the LFA-1 antagonist, lifitegrast (SAR 1118). J Ocular Pharmacol. 2013;29(4):395-402. 31. Zhong M, Gadek TR, Bui M, et al. Discovery and development of potent LFA-1/ICAM-1 antagonist SAR 1118 as an ophthalmic solution for treating dry eye. ACS Medicinal Chemistry Letters. 2012;3(3):203-6. 32. US Food and Drug Administration. FDA approves new medication for dry eye disease. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm510720.htm. Accessed March 23, 2017. 33. Vane JR, Bakhle YS, Botting RM. Cyclooxygenases 1 and 2. Annu Rev Pharmacol Toxicol. 1998;38(1):97-120. 34. Aragona P, Tripodi G, Spinella R, et al. The effects of the topical administration of non-steroidal anti-inflammatory drugs on corneal epithelium and corneal sensitivity in normal subjects. Eye. 2000;14(2):206-10. 35. Hessen M, Akpek EK. Dry eye: an inflammatory ocular disease. Journal of Ophthalmic & Vision Research. 2014;9(2):240-50. 36. Marsh P, Pflugfelder SC. Topical nonpreserved methylprednisolone therapy for keratoconjunctivitis sicca in Sjögren syndrome. Ophthalmology. 1999;106(4):811-6. 37. McGhee CN, Dean S, Danesh-Meyer H. Locally administered ocular corticosteroids. Drug Safety. 2002;25(1):33-55. 38. Celebi ARC, Ulusoy C, Mirza GE. The efficacy of autologous serum eye drops for severe dry eye syndrome: a randomized double-blind crossover study. Graefes Arch Clin Exp Ophthalmol. 2014;252(4):619-26. 39. Pan Q, Angelina A, Marrone M, et al. Autologous serum eye drops for dry eye. Cochrane Database Syst Rev. 2017 Feb 28;2:CD009327. 40. Fox RI, Chan R, Michelson JB, et al. Beneficial effect of artificial tears made with autologous serum in patients with keratoconjunctivitis sicca. Arthritis & Rheumatism. 1984;27(4):459-61. 39. Tsubota K, Goto E, Fujita H, et al. Treatment of dry eye by autologous serum application in Sjögren’s syndrome. British Journal of Ophthalmology 1999;83(4):390-5. 41. Said AM, Farag ME, Abdulla TM, et al. Corneal sensitivity, ocular surface health and tear film stability after punctal plug therapy of aqueous deficient dry eye. Int J Ophthalmol. 2016;9(11):1598-1607. 42. Hom MM, Bruce AS. Prelens tear stability: relationship to symptoms of dryness. Optometry. 2009 Apr;80(4):181-4. 43. Guthrie SE, Jones L, Blackie CA, Korb DR. A comparative study between an oil-in-water emulsion and nonlipid eye drops used for rewetting contact lenses. Eye Contact Lens. 2015;41(6);373-7. 44. Pansell T, Porsblad M, Abdi S. The effect of vertical gaze position on ocular tear film stability. Clin Exp Optom. 2007;90(3):176-81. 45. Acosta M, Gallar J, Bellmonte C. The influence of eye solutions on blinking and ocular comfort at rest and during work at video display terminals. Exp Eye Res. 1999 June;68(6):663-9. 46. Hirota M, Uozota H, Kawamorita T, et al. Effect of incomplete blinking on tear film stability. Optom Vis Sci. 2013 Jul;90(7):650-7. |
