Providing parents with a compelling message to pursue a myopia management modality, all the while working with the confinements of limited exam time, is an exasperating challenge. These discussions require the ability to share sufficient information without overwhelming the patient, to use easy-to-understand terminology while explaining a foreign concept, to convey the value of the treatment plan without push-back on added costs and, most of all, to gain their complete trust in an unfamiliar territory.
The Two Barriers
What verbiage and techniques are necessary to aid in a parent or caretaker understanding that enrollment in your myopia management program is in their child’s best interest vs. continuing along the traditional and less costly route of single vision correction? To answer this question, we need to understand the initial barriers.
Limited education: a myopic eye sees a blurry world, but the world sees the myopic eye no differently. Look at the physical characteristics of two children, one with a refractive error of a -6.00D, and the other with a +0.50D. Would a parent be able to tell the difference? Myopia is easily overlooked as a benign condition, as the eye appears normal. Even if parents have myopia themselves, they are likely unaware of myopia as anything more than a nuisance.
This unawareness stems from the lack of options this generation had available as children. Instead, having their vision progress over time was “fixed” by a stronger prescription each year. One study polled parents on their basic knowledge and feelings towards a child’s diagnosis of myopia. Many parents described myopia as merely an optical inconvenience, an expense, and a cosmetic inconvenience.1
 |
| Use plus lenses to show parents what their child’s vision may look like next year, or even three years later, based on the child’s historical progression and risk factors. Click image to enlarge. |
Limited time: a typical comprehensive exam is too short of a period to provide adequate myopia management education. With managed vision care driving most practices’ revenue, optometrists are required to see anywhere from two to four—or even more—patients per hour. There is inadequate time during an exam to sufficiently explain to a family the importance of myopia management, why they have never heard of it before and what treatment options are available. If any attempts to do so are made, the doctor will have several frustrated patients wanting to get on their way. Most recommendations are to bring the patient back for a consultation; however, mechanisms need to be put in place to determine when that patient will come back and how the doctor will be compensated for their time.
Given these barriers, an impactful, initial discussion on the potential impact of myopia and the treatment options is key. After the initial discussion, the value of clear communication remains vital, as the child enrolls in your myopia management program to enable best practices when handling medical treatments such as atropine 0.05%, multifocals or orthokeratology (ortho-K) at home.
The Six Steps to Success
Having a plan in set can help demonstrate to a parent or caretaker that myopia management should be a priority for their child. Let’s walk through a potential case.
1. Identify candidates in your exam chair. Your technician reviews the next patient with you. “Your 10:00 am patient is an eight-year-old female, Claire. Her uncorrected acuities are 20/150 OD, 20/100 OS.”Before stepping into the exam room with Claire, it is clear by her autorefractor printout and history that she is a young, progressive myope. It is also clear that if single vision correction is prescribed, it is merely a stopgap for the following years, and she will very likely continue to progress. This patient requires myopia management to provide the best standard of care, which is not what her parents are expecting to hear.
In situations like this, be prepared before stepping into the exam room.
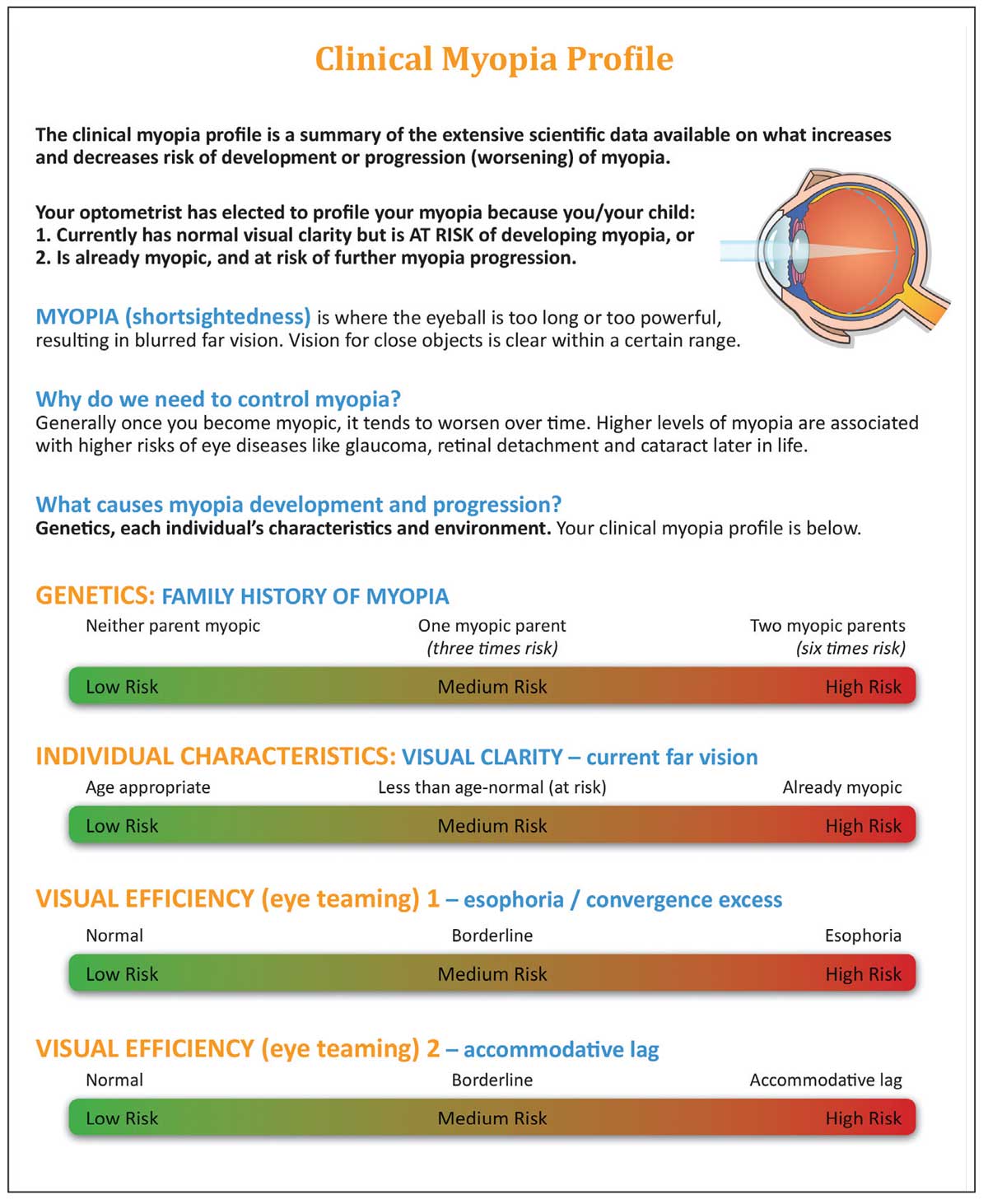 |
| The Myopia Profile tool, designed by Kate Gifford, PhD, helps practitioners explain to the child and their parents the outcomes of the exam more effectively. It is available at www.myopiaprofile.com, along with other resources from Dr. Gifford. Click image to enlarge. |
Train your team to recognize these types of patients as potential candidates for your myopia management program and have educational brochures and pamphlets readily available. They can provide visuals and easy patient verbiage to help improve parent communication.
While establishing history and checking ocular health, get to know the child and parents by asking about hobbies, what they enjoy doing on the weekends, if they are involved in sports, academic clubs, etc. Claire is a member of her swim team.
Start weighing the different modalities of myopia management that are available and what may benefit each patient the most. Specific questions can also help to assess risk factors of a child: Does mom or dad wear glasses? What things do you like to do outside? Do you like playing Minecraft like my niece?
Keep the exam light and fun. It is important to gain the trust of parents and their children by making a positive impression. Be light-hearted and laugh with them to help build a trusting relationship.
2. Express genuine concern and partner with the family. Now it is time for the big discussion, and there is only five minutes of the allotted exam time left. There is simply not enough time to educate them on myopia, the effects of myopic progression, as well as the options that are available. Therefore, it is essential that parents sense your genuine concern, as they will recognize your body language, tone and verbalized concern. The goal is to use this limited time to heighten the parents’ awareness, so they will be driven to pursue a myopia management option.
Start by pulling up a chair next to the parent. Begin by saying, “Claire’s prescription has worsened, and her vision concerns me.” Your body language should mirror the concerned tone of your voice—leaning forward, serious face, slightly elevated eyebrows, etc. Parents may have difficulty comprehending the concepts behind myopia and myopia management, such as why myopia is a concern, how treatments work vs. conventional single-vision correction modalities. Demonstrating genuine concern will motivate the desire to learn more.
Continue by saying, “Claire has progressive myopia, which is a condition that will continue to progress if we continue to prescribe traditional glasses and contacts. This progression will occur until she is much older, typically not stabilizing until her late teens or early twenties.2 I would like to demonstrate to you how she sees the world.”
3. Demonstrate the child’s vision to the family. Show Claire’s myopic vision to her parents by using plus lenses. Ask her parents to step outside of the exam room and look at objects far away. Begin by having the parents hold plus lenses over both eyes that reflect last year’s myopic prescription, then demonstrate the change to the current myopic prescription. Next, show them what their child’s vision may look like next year, or perhaps three years later, based on the child’s historical progression and risk factors. Risk factors may include the age of myopia onset, amount of near work performed each day and parental myopia.3,4,5
Myopia prediction calculators, such as the one created by the Brien Holden Vision Institute, can also be helpful in demonstrating vision changes to parents. Input the child’s age, race, prescription and preferred treatment option into the calculator. Then, demonstrate what the child’s vision may look like three to four years later with vs. without treatment. Parents should be made aware that the calculator overestimates the child’s vision trajectory and data is hypothetical.
Demonstrating vision changes to parents may be more impactful than discussing scare tactics, such as the increased likelihood of ocular disease later in life. This emphasizes that they are occurring now, and these changes are irreversible. It will become clear that their child’s quality of life has been, and will continue to be, negatively impacted. Additionally, parents may feel guilty that they have been unaware of the implications of their child’s vision changes.
“You can see how impactful these vision changes will be over time. If we continue to prescribe regular glasses and contact lenses, this trend will likely continue. The good news is we have options now that have the ability to slow the worsening of Claire’s vision, which can improve her future quality of life and visual potential.”
Based on the parent’s and child’s questions following this short discussion, it will become clear what concerns they have and what guides their motivation, which may be different than anticipated. You can use these questions to drive the conversation in an assuring manner.
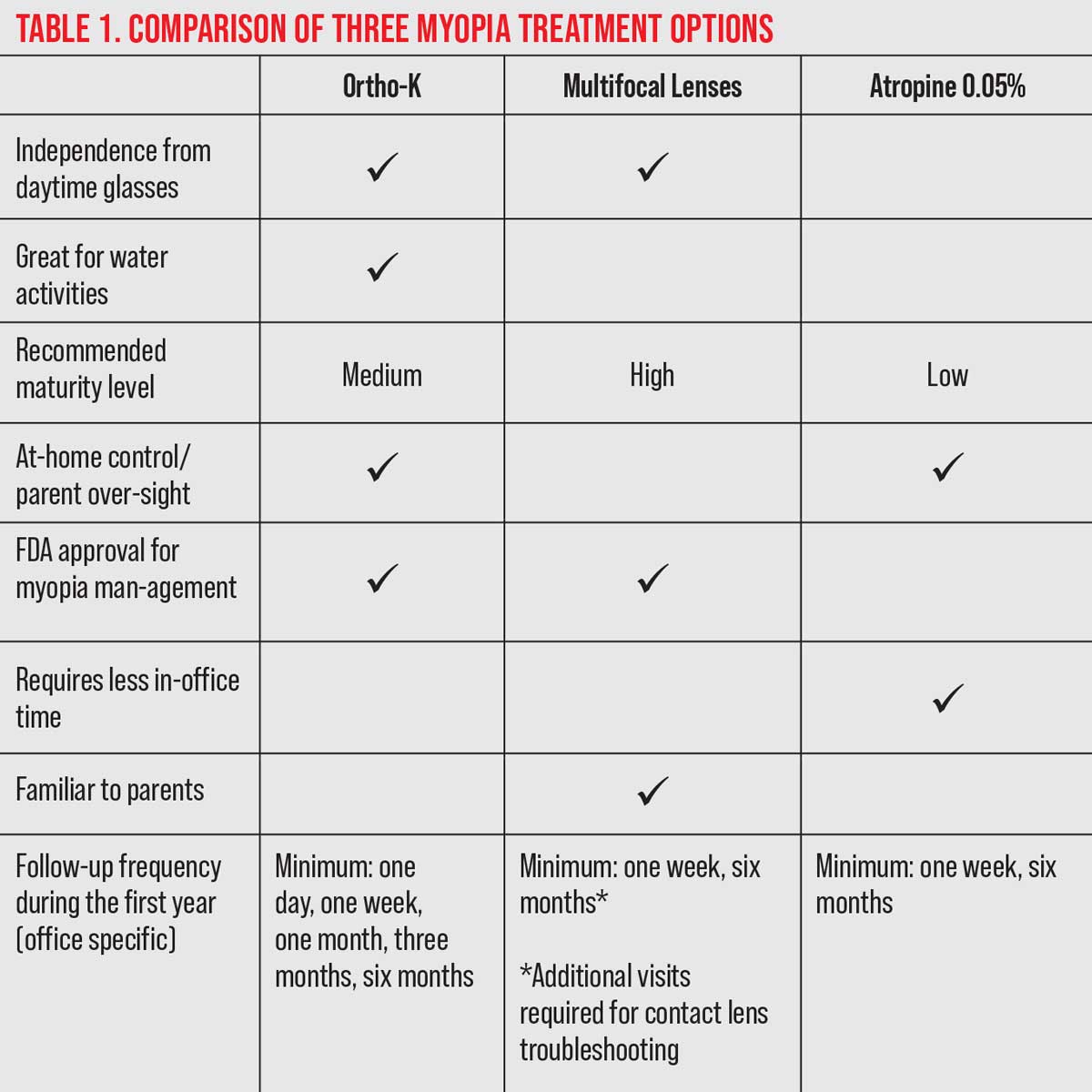 |
| Click image to enlarge. |
It is not necessary to discuss all the details related to myopia and the options available. This limited time is best spent alerting the parent that there is a problem now, you have a solution available and you will work alongside them to improve the child’s vision and quality of life. Quality of life improvements may include a potential increase in self-confidence with contact lens modalities, less visual disability when uncorrected, improved likelihood for refractive surgery candidacy, etc.6 Overall, try to keep it simple, provide resources for review and schedule a consultation.
4. Explain options briefly and schedule consultation. The closing remark could be, “I know this is a lot to take in at once. What are your thoughts on scheduling some time to discuss more after you have had a chance to review our options? Since Claire loves to swim, it appears that the best option may be ortho-K, so that she can be free from contact lenses while swimming. Another contact lens option is a daily disposable contact lens that is worn during the day and disposed of at night. Lastly, an eye drop called atropine can also slow the progression of Claire’s myopia and it is taken nightly. I will provide you with more detailed information on all of these options, so you can all discuss which works best for you as a family. My team will schedule a follow-up visit, either in-person or virtually next week, where we can discuss this condition further. Here is my card if you have any questions before then.”
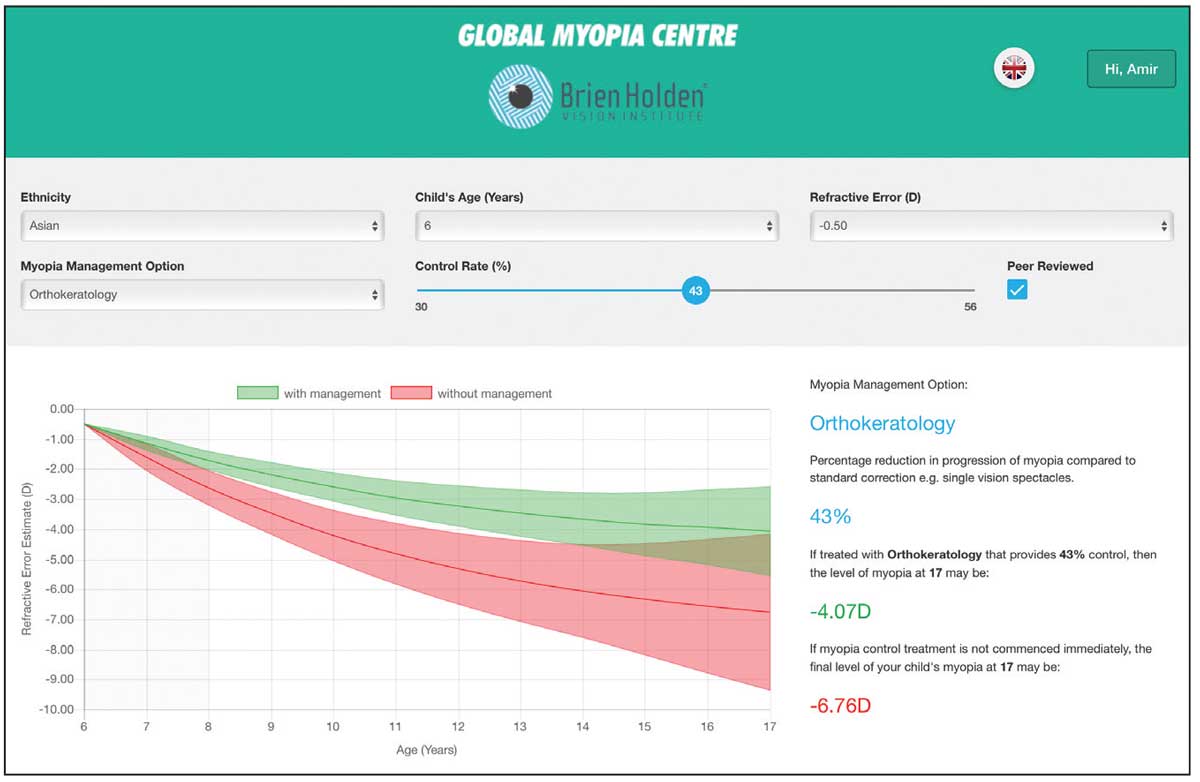 |
| A myopia prediction calculator from the Brien Holden Vision Institute helps demonstrate vision changes to parents. Click image to enlarge. |
It is important that the closing remarks are followed by a call-to-action and a follow-up visit is scheduled. This visit can be in-person or virtual. In addition to providing physical resources, a customized email could be sent to parents outlining your recommendations specific to their child, based on the conversations from the exam. The email should include easy-to-understand websites, videos or graphics on myopia management and addressing frequently asked questions.
5. Drive an effective consultation.
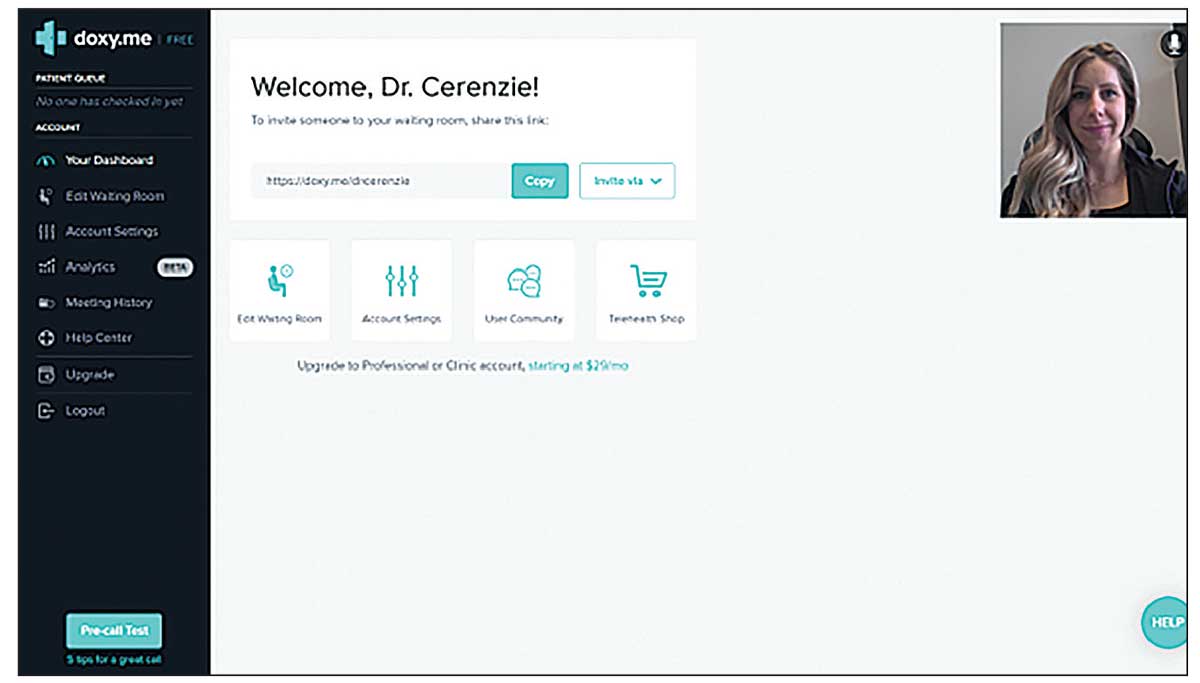
At our office, we perform “tele-reviews” using a HIPAA-compliant telemedicine platform. This has been beneficial to encourage full family participation in the comfort of their own home. In addition, the office is not using resources for the visit. Visits can be scheduled during slow periods or when patients are not being seen. Consider charging for the consult and applying it towards their program if they move forward.
The consult is dedicated to answering all the parents’ questions and concerns. You can easily share resources during the consult. For example, if patients are concerned about safety of contact lenses, send over pertinent literature.7,8
There are several important points to cover. First, assess if the parents appear to understand why myopia management is necessary vs. the traditional, single vision correction route. If there is still some uncertainty, discussions could include:
- Demonstration of the child’s abnormal trajectory of axial length along a growth chart or by using a publicly available refractive error predictor calculator, such as the Brien Holden Vision Institute Calculator.
- Emphasize that, as the child’s prescription increases, their ability to navigate an unfamiliar room decreases. If they were to lose or break their glasses, their function could be significantly impacted until new ones are able to be ordered.
- Discuss the decreased quality of life myopia can bring their child. This includes the need for thicker spectacle lenses annually. In addition to cosmesis concerns, lenses may become more costly as higher index materials will later be recommended. Through higher prescriptions, vision is decreased as objects are minified.
- Awareness that the child may not be a candidate for refractive surgery later in life and, with higher prescriptions, there are higher risks for surgical complications.
- Understanding that with increased levels of myopia, the risk for developing ocular disease also increases.
 |
| A myopia prediction calculator from the Brien Holden Vision Institute helps demonstrate vision changes to parents. Click image to enlarge. |
Parents need to be aware that myopia is certainly more than a nuisance but, potentially, a life-altering condition.
Next, discuss the treatment options the child is a candidate for and what option may be best suited for the child’s lifestyle or hobbies. Discussion could also include the pros and cons of each treatment, frequency of use, expected follow-up frequency and total time expected in office for each visit.
In some studies, there is an association between limited outdoor time and excessive near work with increased myopic progression, though there is insufficient evidence of definitive causation. Unfortunately, there are no specific recommendations for time spent outdoors as it relates to progression, just recommendations on protecting against onset. Until more data is available, it may be helpful to encourage more time outdoors, as well as breaks from prolonged amounts of near work, including screen time. For near work, consider recommending the child holds reading materials or devices further than 30cm and takes breaks after 30 minutes after continuous near-work activity.9,10
Setting the Stage for SuccessIf you were successful with going forward with the ortho-K or the multifocal lens treatment option, there might be another tip that could help those new to contact lens wear: provide them with information on insertion and removal. “We have a little homework for you before coming in for your contact lens class.” Emailing patients and their families videos on lens application and removal, as well as care and handling, may be helpful for few reasons. Watching these videos can help the child feel more comfortable and prepared when the highly anticipated day comes. This will additionally help your technicians’ efficiency, which they will be thankful for. For ortho-K, it may be helpful to instill anesthetic in the eye to decrease the shock of contact lens awareness once initially applied. As the anesthetic wears off, the patient will gradually begin to sense the lenses, as opposed to immediately feeling discomfort. It is critical to emphasize and demonstrate proper lens and hand hygiene at this visit and all subsequent visits.
|
Several reports have found that shorter working distances (<30cm) and continuous near-work activity (>30 minutes) are risk factors for myopia onset and progression.
An example for discussing ortho-K: “These lenses are custom-designed based on Claire’s specific eye shape and prescription. She will be able from daytime correction and free to swim and play without worrying about glasses falling off her face. She will be required to complete an application and removal class, where we will teach her how to safely handle, apply and remove her custom lenses. We will also teach her how to clean her lenses and what specific solutions to use.”
It may be beneficial to warn parents that the application and removal class may take several visits, as the child’s safety is the office’s priority. Lastly, discuss expectations on the follow-up frequency with parents. “Additionally, there will be a minimum of five follow-ups after dispense, one-day, one-week, one-month, three-month and six-month visits. Expect Claire to be here for around 30 to 60 minutes for each follow-up.”
6. Discuss pricing. After the value of the program is understood, then discuss pricing in simple terms. “Our myopia management program is $_____ for the year. The reason is because these treatments require more time and testing than your typical glasses or contact lenses.” It is unnecessary to explain or apologize for the program costs. Discussing larger sums of money may be uncomfortable, but myopia management requires more office time, technology, staff skills and overall, a higher level of care compared with traditional refractive care. The office should be compensated for that, and unapologetically so.
If costs are a concern for patients and their families, dividing the overall sum by monthly payments may be helpful, either directly through the practice or third-party financing. If the office choses to provide the patient with a payment plan without third-party financing, it may be helpful to have a larger sum up front to cover practice costs.
It is beneficial to train your staff on how the fees for myopia management were determined. This will encourage confidence while discussions larger sums of money. One technique is to discuss chair cost with the team, which is the cost it takes to breakeven before the practice profits. The average practice’s chair cost is $136, per the Management & Business Academy (MBA) metrics.11 If a patient has six contact lens follow-up exams, then the practice needs to make a minimum of $816 in services alone to breakeven.
In addition, educate your team on the expense of purchasing a topographer, biometer, additional continuing education and any other necessary tools. When your staff is aware of these expense metrics, the cost structure is more comprehensible, and it will be easier to discuss the costs of myopia management with patients.
Clinical Takeaways
In the future, prescribing myopia management interventions will likely become the standard of care. The World Council of Optometry recently passed a resolution urging optometrists to regularly offer scientifically proven myopia management modalities as the new standard of care for young, progressive myopic patients.12 Until there is widespread recognition of myopia as more than a nuisance—rather, a medical condition amenable to amelioration—education to unexpecting parents and children in-office is imperative.
By demonstrating genuine concern through both body language and verbal communication, parents will be encouraged to pursue your recommendations. Dedicate additional time to continue the myopia management conversation and to continue to provide a clear and effective dialogue throughout the prescribed regimen. Refining communication skills and adjusting our care patterns accordingly are the keys to growing and evolving your myopia management specialty.
Dr. Cerenzie practices at Vision Source Studio 20/20 in Charlotte, NC. She is a Fellow of the American Academy of Optometry and Scleral Lens Education Society. She is also a member of the National Keratoconus Foundation and American Academy of Orthokeratology and Myopia Control. She serves as a key opinion leader for Vision Source’s Myopia Management Protocol. She has no financial interests to disclosure.
|
1. McCrann S, Flitcroft I, Lalor K et al. Parental attitudes to myopia: a key agent of change for myopia control? Ophthalmic Physiol Opt. 2018;38(3):298-308. 2. COMET Group. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54:7871-84. 3. Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children - a systematic review and meta-analysis. PLoS One. 2015;10(10):e0140419. 4. Chua SY, Sabanayagam C, Cheung YB, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36:388-94. 5. Morgan IG, Wu PC, Ostrin LA, et al; IMI risk factors for myopia. Invest Ophthalmol Vis Sci. 2021;62(5):3. 6. Bullimore, MA, Brennan NA. Myopia control: why each diopter matters. Optom Vis Sci. 2019;96(6):463-5. 7. Bullimore MA. The safety of soft contact lenses in children. Optom Vis Sci. 2017;94(6):638-46. 8. Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A three-year randomized clinical trial of Misight lenses for myopia control. Optom Vis Sci. 2019;96(8):556-67. 9. Brennan NA, Cheng X. Commonly held beliefs about myopia that lack a robust evidence base. Eye Contact Lens. 2019;45(4):215-25. 10. Gajjar S, Ostrin LA. A systematic review of near work and myopia: measurement, relationships, mechanisms and clinical corollaries. Acta Ophthalmol. Octoaber 7, 2021. [Epub ahead of print]. 11. Essilor. Key Metrics: Assessing Optometric Practice Performance & Best Practices of Spectacle Lens Management Report. ECP University. 2018. ecpu.com/media//wysiwyg/docs/ECPU_MBA_KeyMetricsReport_2018.pdf. Accessed December 13, 2021. 12. World Council of Optometry. Resolution: the standard of care for myopia management by optometrists. worldcouncilofoptometry.info/resolution-the-standard-of-care-for-myopia-management-by-optometrists. Accessed December 13, 2021. |


