Diabetic macular edema (DME) poses a significant threat to vision, but luckily, the condition is highly treatable. Anti-VEGF injections, the first line of treatment for DME, are effective in most cases, though there is a subset of patients who won’t respond to (or have the means to afford) this ongoing therapy.
“Clinicians may be better prepared to contemplate alternative therapies if they are able to manage treatment expectations and identify patients who are susceptible to a late or inadequate response to treatment,” noted the authors of a new study published in BMC Ophthalmology. In it, they used OCT angiography to detect biomarkers that could predict early anatomical response to DME treatment with intravitreal ranibizumab.
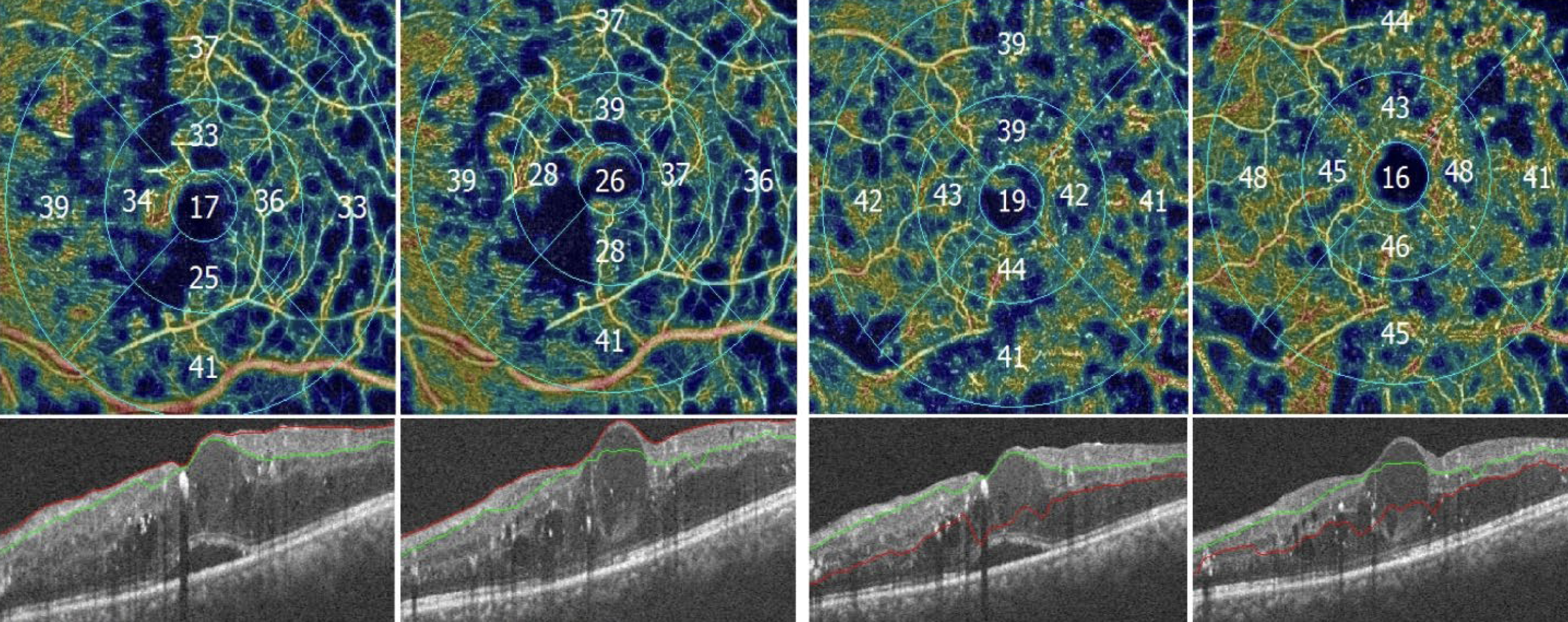 |
| Researchers found that several baseline measurements on OCT-A—specifically the vascular density in the superficial and deep capillary plexuses and FAZ area size—can predict an early-treatment response to intravitreal ranibizumab in DME patients. Photo: Basiony AI, et al. BMC Ophthalmol. 2024;24(429)1. Click image to enlarge. |
The prospective, interventional study examined 111 eyes from 102 patients with DME (59% female; average age: 55), all of whom received three monthly ranibizumab injections. To gauge the effects of therapy, various measurements were compared on OCT-A from before vs. after the treatment course, including central macular thickness, vascular density in the foveal and parafoveal regions and the foveal avascular zone (FAZ) area.
The average BCVA was 0.704 before treatment and improved to 0.305 after treatment in patients who responded well; in those with a poor response, pre-treatment BCVA was 0.66 and changed slightly to 0.54 after treatment. Regarding central macular thickness, good responders showed a reduction from 436.22μm before treatment to 308.12μm afterward, while poor responders showed a change from 387.74μm to 372.09μm.
When examining the FAZ area prior to treatment, good responders had a mean FAZ area of 0.297mm, contrasting with 0.407mm observed in patients who did not respond. The pre-treatment superficial capillary plexus foveal vascular density was higher in good responders at 24.0% compared to 17.9% in poor responders. Similarly, the superficial capillary plexus parafoveal vascular density was also higher in good responders (43.1%) compared to poor responders (37.96%).
Finally, the pre-treatment deep capillary plexus foveal and parafoveal vascular densities were also higher in good responders than poor responders (30.58% vs. 25.45% for foveal; 45.66% vs. 43.26% for parafoveal).
“The superficial and deep capillary plexuses evaluation in OCT-A in conjunction with FAZ area may provide a more accurate prognosis of treatment response and enable earlier management of DME, according to several studies that examined this subject and produced contradictory findings,” the study authors explained in their paper. For example, they noted that prior research found that OCT-A could predict initial anatomical response of DME to intravitreal bevacizumab therapy. An earlier study also identified that the vascular density in the parafoveal area of the superficial layer could predict visual improvement in DME patients following ranibizumab treatment initiated a year earlier. Conversely, another prior investigation found that eyes that responded poorly to anti-VEGF therapy showed considerable damage in the deep capillary plexus integrity, unlike in the superficial capillary plexus, when compared to DME patients who experienced better outcomes. The researchers pointed out that "diverse factors, such as disparate study designs, variations in inclusion criteria and patient characteristics or approaches to image analysis and vascular density quantification, may have contributed to this dispute.”
While larger studies may help clarify these observed relationships between OCT-A parameters and DME treatment response, the researchers summarized, “The vascular density in the superficial and deep capillary plexuses at the macula level, as well as FAZ area size, at baseline can predict an early-treatment response to intravitreal ranibizumab, supporting the belief that eyes with more severe ischemia detected by OCT-A at baseline are less responsive to anti-VEGF treatment.”
| Click here for journal source. |
Basiony AI, Marey HM, Abdel Fattah AME, Zaky MA. Predictive value of optical coherence tomography angiography in management of diabetic macular edema. BMC Ophthalmol. 2024;24(429)1. |

