 |
|
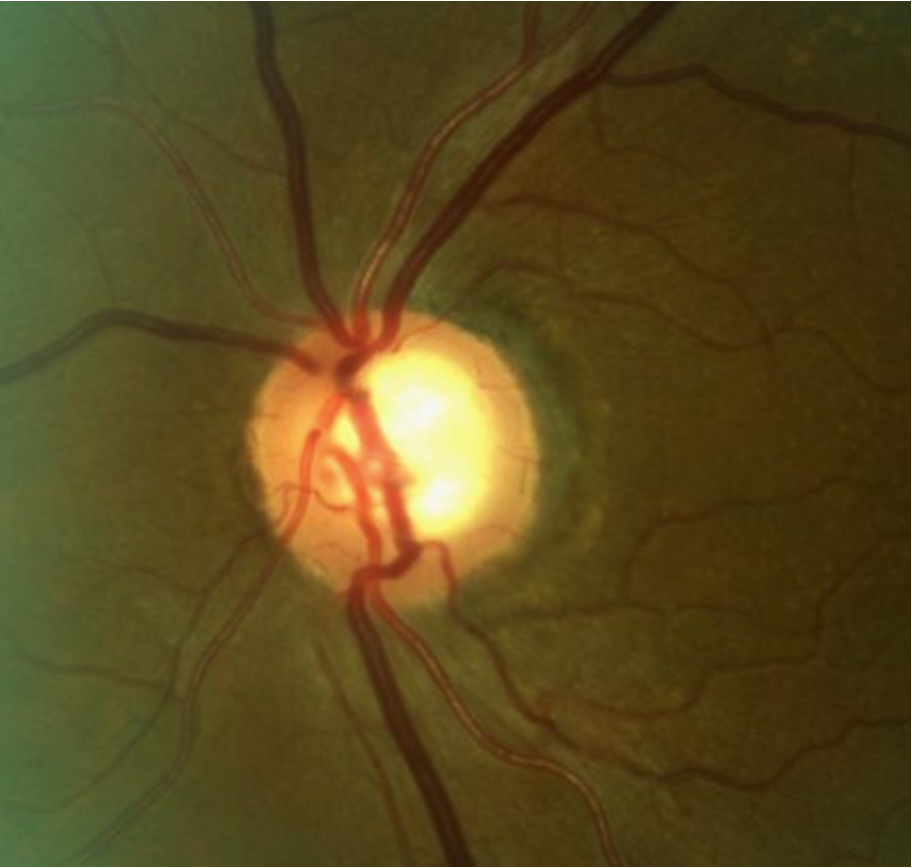
A recent analysis of literature over the past decade highlighted associations between various risk factors and POAG as identified in both cross-sectional and longitudinal studies. Photo: Andrew Rixon, OD. Click image to enlarge. |
To prevent the progression of primary open-angle glaucoma (POAG) and vision loss, early detection and intraocular pressure (IOP)-lowering treatment are crucial. Identifying individuals who are at risk is important for early diagnosis and management. A recent study published in Ophthalmology Glaucoma provided an important overview of recent systematic reviews on the condition, highlighting associations between various risk factors and POAG identified in both cross-sectional and longitudinal studies. Among the reported associations with low risk of bias, the researchers found the highest effect estimates for obstructive sleep apnea and Helicobacter pylori infections in relation to POAG.
Following a full text review of 138 systematic reviews over the past decade, 78 were excluded with reasons, which resulted in 57 reviews. Of these, 30 had a low risk of bias. In the study’s bias assessment, systemic reviews categorized as high risk of bias were characterized by (1) lack of sufficient detail in the bias assessment of the SR and (2) insufficient information or missing calculations of heterogeneity among the included studies.
The research team—with participants from Denmark, Italy and Northern Ireland—identified 22 risk factors associated with POAG with low risk of bias assessment. Among these, the strongest associations with glaucoma (based on effect size) were observed in two systematic reviews related to obstructive sleep apnea, with a pooled odds ratio (OR) of 3.66 and an adjusted OR of 2.46. Similarly, two reviews investigating H. pylori infections showed significant associations, with pooled ORs of 2.08 and 2.08, respectively. Others exhibit more moderate associations, although statistically significant, but were investigated in one systematic review.
When looking at the risk factors identified in the study, the authors pointed out, in their paper for Ophthalmology Glaucoma, that the diversity and apparent variety of potential risk factors present a challenge in finding a single or common cause for the onset of POAG. This diversity emphasizes the multifactorial nature of POAG, where each factor can contribute independently or in combination with other factors.
“Because of this complexity, it is not feasible to propose an overarching hypothesis about the causes of POAG based solely on the findings in this article,” the researchers wrote in their paper.
Nevertheless, the team highlighted their findings in the association of diabetes with POAG, which could “emphasize the need for clinicians to be especially vigilant when monitoring diabetic patients for ocular complications. Additionally, the links between POAG and conditions like sleep apnea, as well as the potential involvement of factors such as statins and H. pylori infections, mandate interdisciplinary communication and collaboration in patient care.”
The study concluded that properly accounting for potential confounders and interactions will provide a more comprehensive understanding of the risk factors involved.
“Employing a variety of research methods, including preclinical models and epidemiological studies, will help refine our understanding of who is at risk and guide the development of more effective prevention and treatment strategies,” the authors emphasized.
| Click here for journal source. |
Rovelt J, Freiberg J, Azuara-Blanco A, et al. The multifaceted non-genetic risk factors for primary open-angle glaucoma – an overview of systematic reviews. Ophthalmol Glaucoma. October 15, 2024. [Epub ahead of print]. |