Scleral Lenses: Boom, Don't Bust
These strategies can help you prevent a scleral lens complication surge in your practice.
By Nurit Ariel Wilkins, OD
Release Date: August 15, 2018
Expiration Date: July 18, 2021
Goal Statement: While scleral contact lenses have traditionally been a last resort for visual correction, they are quickly becoming a first-line option for treatment and vision improvement in many patients with and without ocular disease. With increasing popularity comes an increased risk of adverse events and complications. This article reviews prudent strategies clinicians can implement—such as fitting techniques and following patients with more complex pathology more closely—to manage scleral lens wear while also preventing iatrogenic complications.
Faculty/Editorial Board: Nurit Ariel Wilkins, OD
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 58661-CL. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Authors: The author has no relationships to disclose.
Editorial staff: Jack Persico, Rebecca Hepp, William Kekevian and Catherine Manthorp all have no relationships to disclose.
Scleral contact lenses have become increasingly popular due to improved materials, fitting techniques and more educated practitioners—all of which have led to greater success in patients. While this lens modality has traditionally been a last resort for visual correction, it is quickly becoming a first-line option for treatment and vision improvement in patients with refractive errors as well as with many ocular diseases.
Scleral contact lenses can delay the need for surgical intervention in patients with keratoconus or other corneal ectasias and provide improved vision in patients who have already undergone surgery.1 Likewise, they provide an alternative treatment for ocular surface disease and improved vision and resolution of symptoms in patients who have failed other treatments.2 They also provide excellent visual acuity and comfort in patients with high ametropia.3
While scleral contact lenses create an opportunity to provide patients with optimal vision that would otherwise be unattainable, they also create a great responsibility for practitioners to care for patients with complex ocular diseases. Part of that responsibility includes mitigating the increase in adverse events and complications that can result from the use of scleral lenses. Contact lenses introduce new risk factors to the ocular surface, and clinicians must not only manage the presenting ocular disease, but also prevent iatrogenic complications.
Clinicians should implement the best fitting techniques and follow patients with more complex pathology more closely with evaluation of the ocular surface and the contact lens fit at every visit. Educating patients about their condition, signs and symptoms of potential complications and of proper lens care can also go a long way toward helping prevent adverse events and promote safe scleral contact lens wear.
This article reviews prudent strategies to manage the complexities of scleral lens wear while also preventing iatrogenic complications.
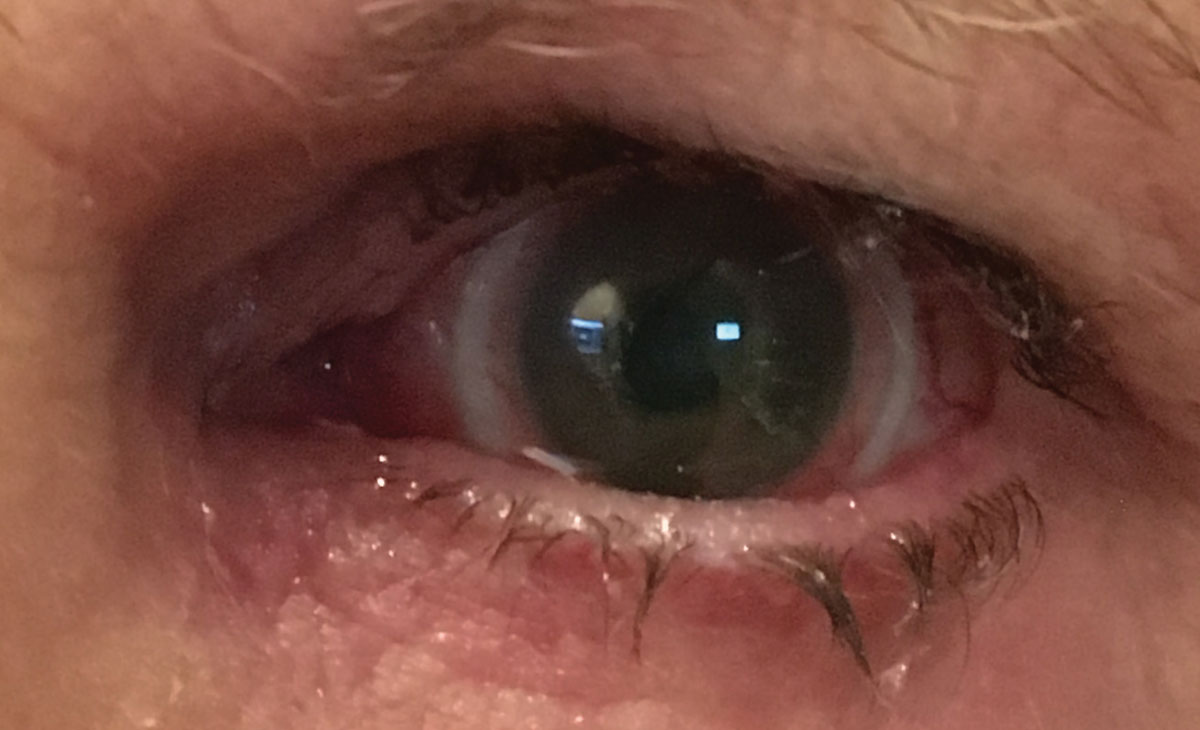 |
| Fig. 1. This scleral contact lens edge is impinging on the conjunctival blood vessels, causing conjunctival blanching and circumlimbal injection. Click image to enlarge. |
Protect the Periphery
With an optimal scleral contact lens fit, the entire edge of the lens lands in alignment with the conjunctival surface without compressing the tissue. It can be difficult to achieve this aligned fit in patients with toric scleral or irregular conjunctival tissue such as conjunctivochalasis, pterygium, pinguecula or a filtering bleb. In fitting patients with complex physiology or pathology, more customized lens options are required to attain an optimal fit.
Irregular conjunctival and scleral surfaces commonly cause poorly fitting scleral landing zones, or haptic zones, by causing the lens to fit too tightly (compressing the conjunctiva) or too loosely (lifting off of the surface of the eye). Poor lens alignment leads to complications such as blood vessel blanching, discomfort, lens fogging, corneal and conjunctival desiccation and conjunctival prolapse. By understanding how to improve edge designs, often by incorporating toric haptics, practitioners can design optimal landing zones and avoid these conjunctival complications.4
Conjunctival blanching of blood vessels. This occurs when the contact lens lands or settles too tightly onto the conjunctival surface, compressing the blood vessels and impinging on blood flow (Figure 1). Blanching may not be evident initially, but can manifest throughout the day as the lens settles, eventually causing redness, circumlimbal congestion and discomfort.5 If lens wear is tolerated despite the poor fit, a compression ring with rebound hyperemia may occur once the lens is removed. Blanching can be sectoral, as commonly seen in patients with toric sclera, or it can occur around the entire haptic zone.
Impingement on the conjunctival blood vessels around the entire haptic zone can lead to lens seal-off, in which the lens becomes excessively suctioned onto the eye and may result in difficult and painful lens removal. Additionally, lens seal-off creates stagnation of the pre-corneal tear and fluid reservoir, which can lead to epithelial toxicity.6,7 Prior to dispensing lenses, contact lens practitioners should optimize the edge design to avoid compressing the conjunctiva. The edge design can be improved by flattening the peripheral curves, increasing the diameter to spread out the landing zone or, in some cases, by reducing the sagittal depth of the lens.
Pterygium. Sectoral impingement can be exacerbated by conjunctival abornomalities such as pterygia or pingueculae. A pterygium is a ‘wing-like’ triangular growth of conjunctival tissue that encroaches onto the cornea.8 Hypertrophy of conjunctival epithelium and subconjunctival connective tissue creates irregular elevation of the conjunctival surface.
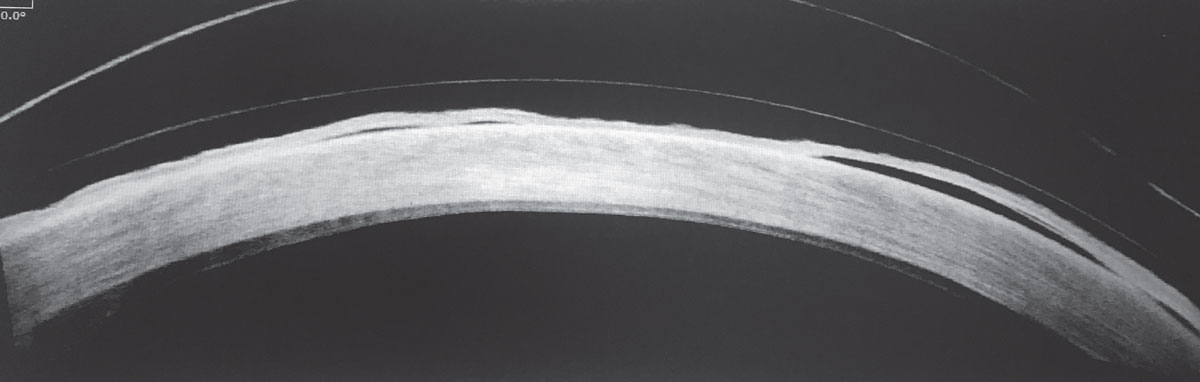
A pterygium induces irregular astigmatism, which cannot always be corrected with spectacles or conventional contact lenses. Scleral contact lenses provide excellent visual correction for patients with irregular astigmatism and therefore are a great choice for patients with pterygia; however, the elevation in the conjunctiva creates an irregular landing zone for scleral contact lenses (Figure 2).9
In these patients, clinicians must be careful to improve the vision without exacerbating the pathology. Pterygia usually occur nasally, causing the scleral contact lens to impinge upon the elevated area.
Patients with chronic conjunctival inflammation or irritation, a potential risk factor for a worsening ptergyium, should wear contact lenses with caution, as poorly fit scleral contact lenses can exacerbate the lesion and accelerate the need for surgical intervention.10
Practitioners can often use lens design strategies to prevent chronic mechanical stimulation or irritation of the elevated conjunctiva. These may include optimizing the diameter, vault, edge design or by implementing a notch into the edge of the lens. For example, selecting a lens diameter that causes the lens to land on the conjunctiva without impinging on the elevated tissue will prevent it from causing irritation or inflammation. Incorporating a notch is another useful technique in which the manufacturer removes part of the edge of the lens to ensure the lens avoids compressing the elevated conjunctiva.5
Lens fogging. When the edge of the lens is too flat and does not land in alignment with the conjunctival surface, the pre-corneal tear layer and fluid reservoir can seep out throughout the day, causing lens fogging and blurry vision, as well as corneal and conjunctival desiccation. Patients often complain of discomfort, as the elevated edges of the lens create a foreign body sensation and rub against the palpebral conjunctiva, causing irritation or papillary conjunctivitis. Clinicians can steepen the peripheral curves to avoid these complications.
Conjunctival prolapse. Conjunctivochalasis is redundant bulbar conjunctival tissue, usually between the limbus and lower eyelid.11 This finding is common in elderly patients and may be associated with thyroid disorder.12 The conjunctival redundancy can lead to symptoms of dryness, tearing, redness, poor lid-globe congruity and poorly fitting scleral contact lenses.12 It can create an uneven landing zone for the scleral contact lens, usually inferiorly, leading to a poorly fitting scleral haptic zone. In addition to disrupting the lens fit, conjunctivochalasis can also lead to conjunctival prolapse, in which the conjunctival tissue becomes trapped under the scleral contact lens.13 This is usually a benign finding, although with prolonged conjunctival prolapse, firm adhesion of the conjunctiva to the corneal surface is possible, which can create a synechia between the cornea and conjunctiva.14
To prevent this complication, patients should be well educated on proper insertion and removal, as well as the importance of an appropriate wearing schedule to avoid over-wearing their contact lenses.
Practitioners should also design a lens with an appropriate vault and landing zone to prevent adhesion between the cornea and conjunctiva. Ensuring proper lens centration can reduce the risk of conjunctival prolapse. To improve centration, practitioners can adjust peripheral curves or incorporate prism ballasts or double slab-off technology. In well-centered lenses with conjunctival prolapse, reducing the overall diameter of the contact lens or reducing the vault over the limbus can help prevent conjunctival prolapse.
In cases where the base curve, vault or edge design cannot prevent conjunctival prolapse, frequent follow-up and monitoring is recommended. Contact lenses should be removed at each visit to allow for manual manipulation of redundant conjunctiva to ensure no adhesion.
If a redundancy of conjunctiva is causing dryness and tearing, artificial tear drops and gels can help manage symptoms. Increasing the vault in the midperipheral or limbal zone can help prevent any prolapsed conjunctiva from adhering to the limbus or corneal surface. In advanced cases that impede safe and comfortable lens wear, referral to an anterior segment specialist for surgical excision of conjunctivochalasis may be necessary.15
Most conjunctival complications can be managed with lens design, good wearing habits and communication with an anterior segment specialist when surgical or advanced medical management is indicated.
 |
| Fig. 2. The edge of this scleral contact lens is landing on a pterygium, causing compression and irritation of the elevated conjunctival tissue. Click image to enlarge. |
A Central Problem
Scleral lens wear can introduce several complications specific to the cornea as well. Here is a look at many of the common issues and how to avoid them.
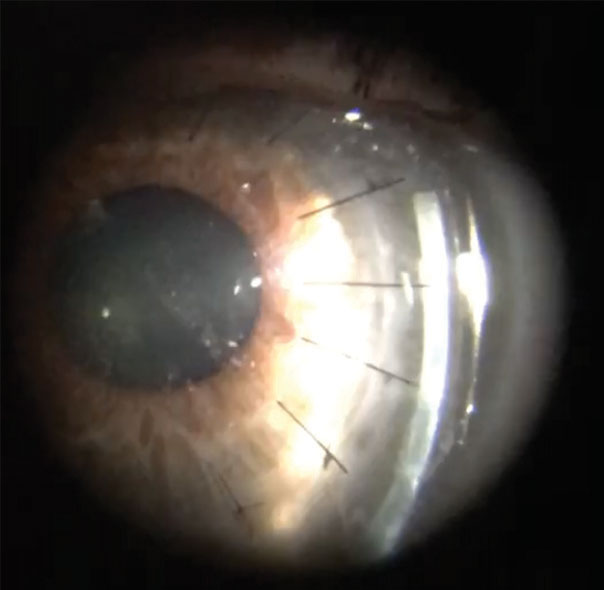
Corneal epithelial staining. This is a complication that should not be seen in healthy scleral contact lens wear because lenses are designed to vault over the cornea without any touch or bearing, but may be seen if lenses are fit with insufficient corneal or limbal vault or if excessive settling takes place. Such a complication can lead to further corneal damage.
Compromised epithelial cells can cause pain and predispose an eye to sight-threatening infection, whereas intact, smooth corneal epithelium protects and defends against microbial keratitis.16 Thus, practitioners should always ensure adequate corneal vault in scleral lenses by assessing the lens fit after complete settling has taken place. Optical coherence tomography (OCT) is a useful tool to accurately assess corneal vault in areas of questionable bearing or touch.17 If there is any bearing seen over the cornea or limbus, the lens should be altered to increase sagittal depth.
Other causes of corneal staining include poorly fit lens edges that cause lens seal-off or lens edge lift, both of which can lead to corneal desiccation. Allergy or sensitivity to the solutions used to clean, store or fill contact lenses can also cause cornea staining.18 Clinicians should carefully educate patients on proper insertion and removal, as corneal abrasion can occur with improper insertion or removal techniques.
Epithelial defects should be well documented and treated until resolution, while non-healing epithelial defects should be referred to a corneal specialist for culturing and evaluation (Figure 3).
Hypoxic corneal changes. In scleral contact lens wear, these are not common; however, complications resulting from hypoxia may be seen with increased frequency as a greater number of patients are fit in scleral contact lenses, and as existing wearers continue to successfully wear their lenses over time. Most hypoxic changes are likely subclinical and benign.5
Bullae, striae and endothelial cell death are not typically associated with contact lens-induced edema, but research is still lacking on the effects of chronic edema over prolonged periods of time.
Acute corneal hypoxia causes corneal edema, which can affect any layer of the cornea. Epithelial edema may be subclinical and result in compromised epithelial integrity and increased risk of microbial infection. Stromal edema causes increased corneal thickness, haze and associated blurry vision. In severe cases, these symptoms can be accompanied by full-thickness edema, hypopyon or frank epithelial defects.19 These changes are uncommon in scleral contact lens wear due to the highly gas-permeable materials used today, but can present in cases of contact lens over-wear, such as overnight wear.20
In cases of extreme corneal hypoxia, lens wear should be discontinued, and symptoms should be treated with prophylactic antibiotics and cycloplegia.20 While lens wear can resume once resolved, clinicians should stress to patients the importance of contact lens compliance, including adhering to the determined wearing schedule.
Chronic corneal hypoxia is also uncommon, but can have serious potential consequences. It can cause changes such as redness, decreased lens tolerance, endothelial cell polymegethism and corneal neovascularization.20 These are more likely to occur in high-powered lenses, which have increased lens thickness, as well as in lower Dk lenses, highly vaulted lenses and with the extended wear modality.
Researchers who have looked at the long-term effects of scleral contact lenses on ocular physiology suggest fitting guidelines to reduce hypoxia: lenses should be designed with highest Dk, least lens thickness and minimal clearance to reduce risk of hypoxia.21,22
Although today’s scleral lenses use highly gas permeable materials and hypoxic complications are rare, tear stagnation in the tear-lens reservoir can lead to epithelial toxicity. One study looked at the permeability of corneal epithelium and found that tear stagnation in overnight contact lens wear decreases the barrier function of the epithelium.6
Limiting wear time and optimizing scleral lens edge designs can prevent tear stagnation and corneal hypoxia, reduce epithelial toxicity and promote healthy scleral contact lens wear.
 |
| Fig. 3. This OCT evaluation of a scleral contact lens in a patient reveals a significant epithelial defect. Click image to enlarge. |
Keep the Bugs at Bay
Microbial keratitis is a rare, but potentially devastating, complication of scleral contact lens wear. While uncommon, it could become a more widespread problem as scleral contact lenses become more popular, as contact lens wear is the most common predisposing factor for microbial keratitis.23 Other risk factors for microbial keratitis include ocular surface disease, prolonged steroid use and decreased corneal sensation.23
Corneal infections should be detected early and treated promptly with appropriate medication to prevent permanent vision loss. Referral to a cornea specialist should be considered for management, including obtaining microbial culture and treatment with antibiotics.16
Contact lens hygiene is an easily modifiable risk factor, and adherence to healthy habits and use of appropriate solutions can reduce the risk of infection. The best way to prevent permanent vision loss from bacterial keratitis is to avoid contact lens over-wear and to educate patients regarding the importance of good contact lens hygiene.24
Ocular surface disease is one of the most common indications for scleral contact lens wear, further promoting the modality’s popularity. Patients with ocular surface disease can experience improved vision, as well as resolution of keratopathy with the use of scleral lenses.2 However, in treating ocular surface disease with scleral contact lenses, practitioners should be aware of the risks of infection in patients with keratopathy, thoroughly assess for signs of early infection even in the absence of symptoms, and consult a cornea specialist when needed.
 |
| Fig. 4. Evaluation of a scleral contact lens with optic section reveals variation in elevation over the graft-host junction with sutures intact. |
Many patients require long-term steroid use as part of their disease or postoperative management and are therefore at increased risk for microbial keratitis. Decreased corneal sensation may be common in patients who have undergone corneal surgery, or who have previous history of corneal herpetic infection. These patients often require scleral contact lenses for ocular surface protection, as well as for visual correction, but are at higher risk for infection due to hypoesthesia. Increased monitoring and exceptional patient education can reduce the risk of ocular infection in these patient populations.
To prevent a surge in microbial keratitis, practitioners should prioritize patient education to encourage safe and hygienic behavior from their patients.25,26
After the Cut
The most common indication for fitting scleral contact lenses is keratoconus.27 Corneal transplantation, specifically penetrating keratoplasty (PKP), is a full-thickness corneal transplant that is often the best treatment to restore vision in advanced keratoconus. This surgery has been considered a safe and effective treatment for corneal ectasia and scarring for more than one hundred years.28
PKP frequently results in significant amounts of astigmatism, which makes it difficult to achieve satisfactory visual acuity even once the eye has healed. Despite optimal surgical outcomes, many patients are left with poor vision due to high corneal toricity. When fit correctly, scleral contact lenses can provide safe and non-invasive treatment for refractive error and post-keratoplasty astigmatism and can prevent the need for additional ocular surgery.
In fitting scleral contact lenses post-PKP, the goals are the same as in any other successful fit: clearing the cornea and the limbus without excessive vault and landing in alignment with the conjunctival surface. However, transplanted corneas present more challenges due to significant differences in elevation between the donor and host graft. Edema at the graft-host junction presents an additional challenge because of increased elevation and irregularity. Another fitting challenge is the complex topography and variation in corneal graft shapes, with some being prolate, some oblate and some a unique combination.1 Practitioners should avoid an excessively thick tear reservoir to allow for adequate oxygen permeability, as this is necessary for graft survival.
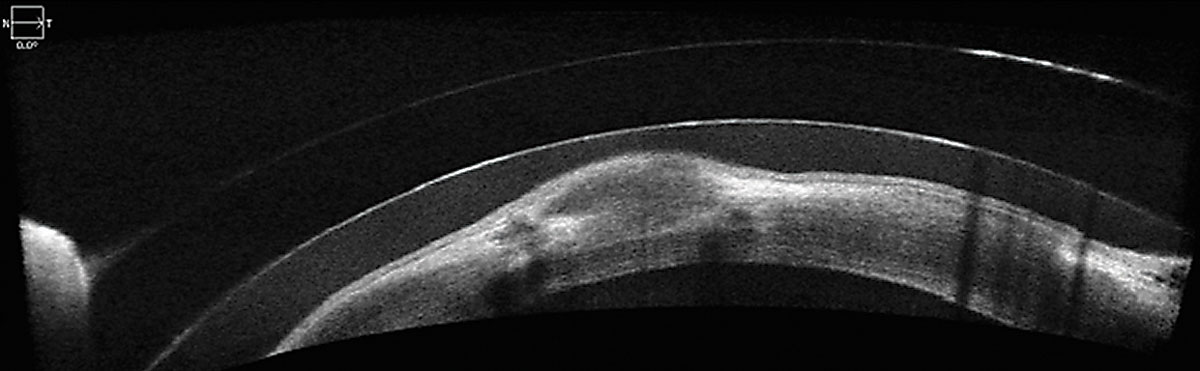 |
| Fig. 5. Evaluating a scleral contact lens fit with OCT reveals clearance over the edematous graft-host junction. Click image to enlarge. |
Failure to achieve an adequate fit can cause corneal hypoxia, edema, neovascularization and infection, and can lead to graft rejection. When sutures remain in place, the graft-host junction requires extra evaluation for loose or broken sutures, overlying epithelial staining or subepithelial infiltrates (Figures 4 and 5). If any signs of suture abscess or infection are seen, lens wear should be discontinued, and the patient should be referred back to the surgeon.
To prevent a surge in complications in patients who have undergone corneal transplantation, an optimal fit should be achieved, followed by close monitoring. It is important to educate the patient extensively about signs and symptoms of corneal graft infection and rejection. Practitioners should look for signs of corneal graft rejection at every visit and ensure the contact lenses are not causing any corneal insult that could lead to rejection.
In comanaging post-PKP patients, practitioners should be vigilant in assessing for complications such as infectious crystalline keratopathy, herpetic epithelial disease, glaucoma, cataract and suture abscess.28 It is important to identify signs of rejection early and treat aggressively by discontinuing lens wear, adjusting necessary parameters, initiating steroid treatment and referring back to the surgeon as needed.
Scleral contact lenses have extensive indications for visual correction and management of complex ocular diseases, making them an excellent option, for both practitioners and patients. Often the ocular pathology requires comanagement with an anterior segment specialist to prevent complications or worsening of disease. As contact lens practitioners, it is important to understand the ocular pathology being treated, the risk factors for complications and the signs to evaluate for at each follow-up visit.
By fitting scleral contact lenses with appropriate clearance over the entire cornea and limbus and proper alignment with conjunctiva, we can prevent complications such as corneal staining and hypoxia. Practitioners have a responsibility to educate patients on lens hygiene, appropriate solutions and potential symptoms of complications. Each of these strategies can go a long way to prevent any potential surge of complications with the increase in popularity of scleral contact lenses.
Dr. Wilkins is a graduate of the Pennsylvania College of Optometry at Salus University, where she went on to complete her residency in cornea and specialty contact lenses. She practices in Baltimore, MD.
1. Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: Long term outcomes. Contact Lens Ant Eye. 2014;37(3):196-202. 2. Schornack MM, Pyle J, Patel SV. Scleral lenses in the management of ocular surface disease. Ophthalmology. 2014 Jul;121(7):1398-405. 3. Nau A, Nau C, Shorter E, et al. SCOPE study: indications for scleral lens wear. Poster presented at the 2016 Global Specialty Lens Symposium, January 2016, Las Vegas, NV. 4. Visser ES, Van der Linden BJ, Otten HM, et al. Medical applications and outcomes of bitangential scleral lenses. Optom Vis Sci. 2013;90(10):1078-85. 5. van der Worp E. A guide to scleral lens fitting [monograph online]. Scleral Lens Education Society. 2010. http://commons.pacificu.edu/mono/4/. Accessed June 25, 2018. 6. Walker MK, Bergmanson JP, Miller WL, et al. Complications and fitting challenges associated with scleral contact lenses: A review. Cont Lens Anterior Eye. 2016 Apr;39(2):88-96. 7. Lin MC, Polse KA. Hypoxia, overnight-wear, and tear stagnation effects on the corneal epithelium: data and a proposed model. Eye Contact Lens. 2007 Nov;33(6 Pt 2):378-81. 8. Duke-Elder S. Diseases of the outer eye. Syst Ophthalmol. 1965;8:573-85. 9. Tan D, Chan C. Management of pterygium. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St. Louis, Mo: Mosby/Elsevier; 2011:1625-40. 10. Coroneo MT, Di Girolamo N, Wakefield D. The pathogenesis of pterygia. Curr Opin Ophthalmol. 1999 Aug;10(4):282-8. 11. Murube J. Characteristics and etiology of conjunctivochalasis: historical perspective. Ocul Surf. 2005 Jan;3(1):7-14. 12. Meller D, Tseng SC. Conjunctivochalasis: literature review and possible pathophysiology. Surv Ophthalmol. 1998 Nov-Dec;43(3):225-32. 13. Jedlicka J. Solving scleral lens complications. Contact Lens Spectrum. 2012 October;27:40-4. 14. Andre C, Andre M. Contact lens case reports: a potential effect of conjunctival prolapse. Contact Lens Spectrum. 2013 September;28:56. 15. Rapuano CJ. Surgical management of superficial corneal and conjunctival disease. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St. Louis, Mo: Mosby/Elsevier; 2011:1606. 16. Edelstein S, Wichiensin P, Huang AJW. Bacterial keratitis. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St. Louis, Mo: Mosby/Elsevier; 2011:919-44. 17. Sorbara L, Maram J, Fonn D, et al. Metrics of the normal cornea: anterior segment imaging with the Visante OCT. Clin Exp Optom. 2010;93:150-6. 18. Gromacki SJ. A how-to guide: scleral GP lens care. Review of Cornea and Contact Lenses. 2013 January-February;150(1):22-24. 19. Cohen EJ. Complications of contact lens wear. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St. Louis, Mo: Mosby/Elsevier; 2011:1231-8. 20. Smith GT, Mireskandari K, Pullum KW. Corneal swelling with overnight wear of scleral contact lenses. Cornea. 2004;23:29-34. 21. Michaud L, van der Worp E, Brazeau D, et al. Predicting estimates of oxygen transmissibility for scleral lenses. Contact Lens Anterior Eye. 2012;35:266-71. 22. Compan V, Oliveira C, Aguilella-Arzo M, et al. Oxygen diffusion and edema with modern scleral rigid gas permeable contact lenses. Invest Ophthalmol Vis Sci. 2014;55:6421-9. 23. Bourcier T, Thomas F, Borderie V, et al. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. British J Ophthalmol. 2003;87:834-8. 24. Alipour F, Khaheshi S, Soleimanzadeh M, Heidarzadeh S, Heydarzadeh S. Contact Lens-related complications: a review. J Ophthalmic Vis Res. 2017 Apr-Jun;12(2):193-204. 25. Stapleton F, Carnt N. Contact lens-related microbial keratitis: how have epidemiology and genetics helped us with pathogenesis and prophylaxis. Eye (Lond). 2012 Feb;26(2):185-93. 26. Fleiszig SM, Evans DJ. Pathogenesis of contact lens-associated microbial keratitis. Optom Vis Sci. 2010 Apr;87(4):225-32. 27. Nau A, Nau C, Shorter E, et al. SCOPE study: indications for scleral lens wear. Poster presented at the 2016 Global Specialty Lens Symposium, January 2016, Las Vegas, NV. 28. Miller CA, DeMill DL. Routine management. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St. Louis, Mo: Mosby/Elsevier; 2011:1336. 29. Foulks G. Diagnosis and management of corneal allograft rejection. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St. Louis, Mo: Mosby/Elsevier; 2011:1409-16. 30. Price MO, Jordan CS, Moore G, et al. Graft rejection episodes after Descemet stripping with endothelial keratoplasty: part two: the statistical analysis of probability and risk factors. British J Ophthalmol. 2009;93:391-5. |
