Keratoconus Risk Factors Revealed
The largest study ever on this disease uncovers some surprises about who may—or may not—be at an increased risk.
By Rebecca Hepp, Senior Associate Editor
A recent retrospective, longitudinal cohort study has discovered associations between certain sociodemographic factors, common systemic diseases and the risk of keratoconus (KCN). Researchers at the University of Michigan Health System’s Kellogg Eye Center and the U-M Institute for Healthcare Policy and Innovation matched 16,053 patients with KCN 1:1 with patients without KCN using billing codes, age, gender and overall health to discover if certain sociodemographic factors and systemic diseases affected the odds of KCN.
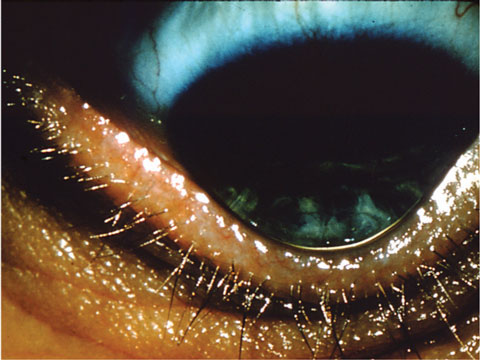 |
| Data from over 32,000 subjects reveals several risk factors for keratoconus. Photo: Maria Woodward, MD. |
“This study is the largest study ever on keratoconus, with over 32,000 subjects,” says Andrew Morgenstern, OD, an executive board member of the International Keratoconus Academy of Eye Care Professionals. “This was amongst a large, diverse group of insured individuals; these people have the capability of getting treatment, so these are patients in the chair.”
The results of the study show black and Latino patients are at a 57% and 43% increased risk of KCN, respectively, compared with whites, while Asian patients have a 39% reduced risk of a KCN diagnosis compared with whites.
As for systemic diseases, the researchers discovered patients with diabetes mellitus or collagen vascular disease have 20% and 35% lower odds, respectively. Those diagnosed with sleep apnea, asthma and Down syndrome were at increased risk.
The study should have a significant impact on clinical practice, Dr. Morgenstern says, considering it identifies specific patient populations that have to be counseled when they are in the office.
“This study is fantastic because it has such a large sample size and it clearly identified common risk factors and sociodemographic issues,” Dr. Morgenstern says. “Now that it’s out there, it will affect the standard of care for keratoconus screening.”
“For example, because of the high rates of obesity in the United States, and because allergens in certain areas of the United States are high, there are higher populations with sleep apnea and asthma now,” Dr. Morgenstern says. “The study suggests that if patients have these breathing issues, they have to be counseled on the higher risk of keratoconus.”
“As eye care providers, we are qualified to diagnose keratoconus, but a patient with keratoconus should be aware of other conditions that may affect their overall health,” says Maria Woodward MD, an assistant professor of ophthalmology at the U-M Medical School and first author of the new study. “We believe the most important thing for practicing eye care providers is to ask about sleep apnea risk factors and asthma for patients with keratoconus.”
These findings could go a long way toward improving not only patient education, but also the possibility of newer treatment options, such as corneal crosslinking.
“This study will help promote the understanding of corneal collagen crosslinking and how important it is that the FDA approve this procedure,” Dr. Morgenstern says. “If you can identify keratoconus early enough and crosslink it early enough, you can prevent the vision loss in these patients.
“I believe Dr. Woodward and her group at the University of Michigan did a great service to the ongoing understanding of this all too common disease of the cornea,” Dr. Morgenstern says.
Woodward MA, Blachley TS, Stein JD. The Association Between Sociodemographic Factors, Common Systemic Diseases, and Keratoconus: An Analysis of a Nationwide Heath Care Claims Database. Ophthalmology. 2015 Dec 16. [Epub ahead of print].
Researchers at Case Western Reserve University School of Medicine, funded by the National Eye Institute (NEI), part of the National Institutes of Health, recently discovered three genes associated with primary open-angle glaucoma (POAG)—possibly opening the door to future advancements in its detection and treatment.
Using data from the NEI Glaucoma Human Genetics Collaboration Heritable Overall Operational Database, investigators compared the DNA of 3,853 people with POAG with 33,480 controls and found that variations in the FOXC1, TXNRD2 and ATXN2 genes were associated with POAG.
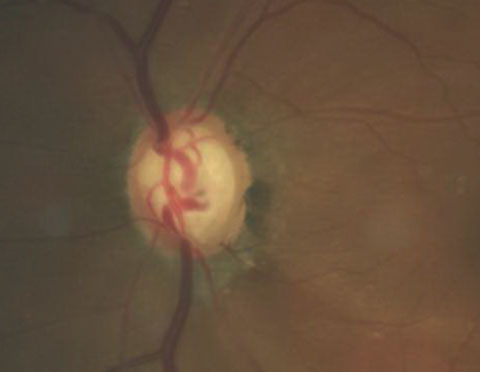 |
| Photo: Joseph W. Sowka, OD. |
FOXC1 had previously been associated with rare cases of severe-onset glaucoma, according to a press release, but the TXNRD2 and ATXN2 associations were a surprise. TXNRD2 helps protect mitochondria against oxidative stress, and its association with POAG “is the first direct report to show the association of a gene linking oxidative damage to glaucoma,” Neeraj Agarwal, PhD, a program director at NEI, said in a press release.
Researchers also discovered both TXNRD2 and ATXN2 are expressed in retinal ganglion cells and the optic nerve head.
“This is a strong step forward to better understanding not only the genetic component of POAG, but also the potential of mitochondrial oxidative stress in the overall pathophysiology of the disease,” says Joseph W. Sowka, OD, professor, chief of the Advanced Care Center and director of the Glaucoma Service at Nova Southeastern University College of Optometry. “But it is only a step along our pathway of understanding.”
While study authors hope the findings will lead to new therapies, Dr. Sowka has concerns that “once this is widely known, there may be financial incentives for companies to develop a genetic test for glaucoma,” he says. “Not very long ago there was a genetic test for glaucoma that imparted very little useful information to assist with the clinical care of patients and it quietly vanished.” But, “at some time in the future, we may have a better understanding of glaucoma genetics and true targeted gene therapy may then become possible,” Dr. Sowka says.
Bailey JNC, Loomis SJ, Kang JH, et al. Genome-wide association analysis identifies TXNRD2, ATXN2 and FOXC1 as susceptibility loci for primary open-angle glaucoma. Nature Genetics. 2016. DOI: 10.1038/ng.3482.
Patients diagnosed with glaucoma may be subjected to increased intraocular pressure (IOP) while practicing yoga, particularly during positions in which the head is facing downward, according to researchers from the New York Eye and Ear Infirmary of Mount Sinai.
Patients are encouraged to remain active; however, patients with glaucoma should avoid exercises that could increase IOP such as pushups and lifting heavy weights, said Robert Ritch, MD, senior author of the study, in a press release.
“This new study will help clinicians advise their patients on the potential risk associated with various yoga positions and other exercises that involve inverted poses,” Dr. Ritch said.
The study compared the IOP of 10 healthy patients with 10 patients with glaucoma while performing several head-first yoga positions, including standing forward bend, downward facing dog, plow and legs up the wall. The researchers measured baseline IOP, then took measurements after having the groups hold the poses briefly, for up to 120 seconds and during seated resting times of up to 10 minutes.
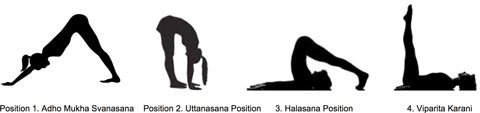 |
| Subjects performed several yoga positions, including downward facing dog, standing forward bend, plow and legs up the wall. Image: PLOS ONE. |
Measurements of both participant groups revealed a rise in IOP in all of the yoga positions tested, and downward facing dog showed the greatest increase in pressure— IOP increased from 17mm Hg to 28mm Hg in glaucoma patients and 17mm Hg to 29mm Hg in normal patients, according to the study. All yoga poses were associated with a significant increase in IOP within 60 seconds of taking yoga positions and returned to normal within two minutes of returning to the seated position.
Because elevated IOP is an important risk factor for further nerve damage, “the rise in IOP after assuming the yoga poses is of concern for glaucoma patients and their treating physicians,” said first author and doctoral student Jessica Jasien, in a press release. She suggested glaucoma patients share their diagnosis with their yoga instructors to allow for proper modification during practice.
Although the study suggests certain aspects of yoga are a cause for concern, some optometrists remain uncertain regarding its clinical impact. “Certain activities do increase IOP while performing them,” says James Fanelli, OD, of Cape Fear Eye Institute in Wilmington, NC. “For instance, if you wore a tight necktie 24/7 or were inverted 24/7, then that can realistically increase risk. But activities limited in duration probably do not pose significant risk long-term; however, this would be helpful in cases when a patient is continuing to worsen despite an aggressive treatment approach.”
Jasien JV, Jonas JB, de Moraes CG, Ritch R. Intraocular pressure rise in subjects with and without glaucoma during four common yoga positions. PLOS ONE. 2015 Dec. doi:10.1371/journal.pone.0144505.
In the news
Researchers have found a rare link between the varicella zoster vaccine and corneal inflammation. A review of case studies, presented at the 2015 meeting of the American Academy of Ophthalmology, discovered 20 cases of keratitis that developed within a month of administration of the vaccine.
Saskatchewan Health Minister Dustin Duncan will allow ODs to independently treat glaucoma, against the advice of the College of Physicians and Surgeons. The College feels treatment should be done collaboratively with ophthalmologists, according to associate registrar Bryan Salte in a press release. However, Mr. Duncan is satisfied the Saskatchewan Association of Optometrists (SAO) will ensure members remain up-to-date on necessary training—98% are already compliant with recertification.
| Correction In the article, “ACA Children’s Vision Health Benefit: Boom or Bust?” (December 2015), the American Optometric Association was mislabeled as the American Academy of Optometry. The first “Call To Action” point should have read: “Work with the American Optometric Association’s (AOA) ‘Think About Your Eyes’ and ‘InfantSEE’ programs to publicize the importance of eye health in your community.” |
The Multi-Ethnic Pediatric Eye Disease Study (MEPEDS), the largest study of childhood eye diseases ever undertaken in the United States, confirms that childhood myopia among American children has more than doubled over the last 50 years, according to a news release. The study was conducted by researchers from the USC Eye Institute at Keck Medicine at USC in collaboration with the National Institutes of Health (NIH).
Researchers at Boston Children’s Hospital recently restored some vision in mice with optic nerve injury by using gene therapy in combination with a drug cocktail. They are now testing whether injecting the cocktail of growth factor proteins directly into the eye could be equally as effective as the gene therapy alone.
