The Lowdown on Low Vision
Don’t be so quick to write off its business viability, readers argue.
|
Low Vision Can Flourish in Private Practice
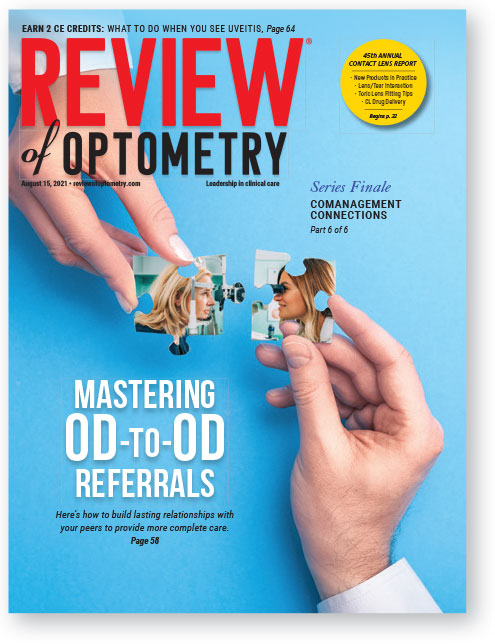
The August issue contains an excellent article on intraprofessional collaboration called, “Mastering OD-to-OD Referrals,” which includes a section on the importance of addressing low vision with every affected patient. Thank you for raising awareness of the need for more low vision care, whether provided directly or comanaged with a doctor suitably skilled for it.
However, there is a comment in the low vision discussion that is, in our opinion, inaccurate. A doctor states that “proper low vision care is time-consuming and very difficult to fit into a private practice model.” The International Academy of Low Vision Specialists (IALVS), established in 2006, has 40 low vision optometrists throughout the United States and Canada who are in private practice. All of our doctors are fully trained and experienced to provide low vision care and rehabilitation in the private practice setting.
—Richard J. Shuldiner, OD, FAAO
President, International Academy of Low Vision Specialists
Clinical Director, Low Vision Optometry of Southern California
Low Vision Diplomate Emeritus, American Academy of Optometry
Vision Rehab Can Set a Practice Apart
Reading the feature, “Mastering OD-to-OD Referrals,” I was blown away by some of the opinions regarding low vision—and not in a good way.
There’s a comment stating that most low vision services are offered today at academic and non-profit institutions rather than in private practice and that this isn’t likely to change “until insurance reimbursement structures for low vision devices and services are altered to lessen the time and financial burdens that make it impractical for private practice ODs to take part.”
My wife, Dr. Lynne Noon, and myself are 1982 graduates of the New England College of Optometry. I chose a career in commercial optometry while Lynne chose vision rehabilitation and subsequently achieved Diplomate status in the discipline of low vision.
She started her solo practice from scratch doing only vision rehab. She spent countless hours meeting with state agencies and other vision rehabilitation experts. She traveled throughout Arizona and the surrounding Southwest region doing low vision exams and lecturing to support groups, optometrists and other medical professionals. Through her hard work and that of others, she helped Arizona adopt biopic driving privileges.
We have both recently retired. But here’s the kicker! It literally took years to find someone to purchase our practice even though it grossed over $2 million annually. What does that say about our profession? The medical model is being taught and pushed to practitioners, yet insurance reimbursements are not adequate. The key to any successful business is to provide a service no one else provides and, better yet, a business that doesn’t rely on insurance reimbursement for products.
Low vision rehabilitation currently meets those two criteria.
The “social welfare model” for low vision care is ancient history. Do not assume these patients are poor and unable to pay for such products and services.
And, as has been proven time and time again, insurance companies are not our friends! We rely on them at our own peril—and our patients’ too.
—Robert Kanocz, OD
Mesa, AZ
From the Editor: The experience of Dr. Shuldiner and his colleagues in the IALVS does show that low vision can thrive in private practice. However, it’s not a contradiction to also acknowledge that ramping up a practice devoted to such care—and ensuring such patients receive the additional time and attention that a typically frail population requires—can be time-consuming and, to many, intimidating.
Dr. Kanocz’s anecdote about the difficulty he encountered selling his practice seems to document that widespread hesitation does exist among individual doctors and/or investors. Rightly or wrongly, there’s at least a perceived barrier to entry. We thank both letter-writers for modelling success in this important area of care. Let’s hope others follow in their footsteps.
|
Who Defines What Constitutes an “Expert”?
I read the article, “Keep Glaucoma Care Close to Home,” in the July 2021 issue with interest. Well done!
One comment: Dr. Danica Marrelli is referred to in the piece as a “glaucoma expert.” I believe such a reference is subjective and borderline inappropriate. Instead, Dr. Marrelli’s accomplishment as a Clinical Diplomate in the Glaucoma Section of the American Academy of Optometry should have been the salient distinguishing credential that documents her “expertise,” which she most certainly possesses.
As optometry moves toward clear recognition of subspecialization (as discussed at length in your October 2020 issue), it should be the goal to recognize appropriate “expertise” that is certified by a body of similar subspecialists (i.e., the Academy Diplomate program).
Thank you for the great service you provide to the profession.
—Jeffrey C. Krohn, OD, FAAO
Fresno, CA
Diplomate, American Board of Optometry and American Academy of Optometry
Chair, AAO Section on Cornea, Contact Lenses & Refractive Technology
Administrator, Vision Source
From the Editor: The above perspective is an interesting one, but the need for precision in discussing credentials may be more acute in messages the public sees rather than those within the optometric community.
Patients need credible resources that direct them to the best doctor for their condition. As discussed in the October 2020 article mentioned by Dr. Krohn, any OD can choose to self-identify as a “specialist” or an “expert” if they feel justified in doing so. There’s at least the potential for patients to wonder about the basis for such a claim.
By contrast, within the profession experts like Dr. Marrelli are well-recognized as such, so we frequently do use the shorthand descriptions “specialist” and “expert” without elaboration—as a matter of brevity and a nod of respect.
Still, we do see the value of conveying more fully the accomplishments of our contributors and will make the effort to do so in the future. In fact, we’ve already started: the letters here from Dr. Krohn and Dr. Shuldiner both list their professional affiliations in detail.
Stop Ignoring Third-party Plans
A recent letter entitled, “Low Marks for Low Vision,” in July 2021 voiced concerns about the lack of sufficient coverage for that important topic.
I’d like to add another low mark for neglected coverage—this time about third-party vision plans and the damage they do to our profession. These plans and their administrators, oppressive fee schedules and complex Explanation of Benefits rules dominate our profession and consume most of our office time, but the optometric press is woefully deficient in providing any articles, discussions, criticism or even praise for these companies and their policies.
Throughout the years, I have often petitioned numerous publications to address this vital part of practice, only to have such calls fall on deaf ears. My suggestion was to create an open forum that would include a monthly article by an OD or a vision insurance executive, with printed responses from readers.
Review is the premier journal for our profession. Its articles are superb, and it keeps us well informed. It is my hope that Review would give serious consideration to this suggestion.
—Alan Frank, OD
Kingston, PA
From the Editor: We thank Dr. Frank for his praise as well as his criticism. The topic of third-party plans is certainly on the minds of many ODs, and we welcome the opportunity to enable conversation about it right here—in our Letters to the Editor section. Readers who wish to share anecdotes, gripes, success stories, horror stories or anything else are encouraged to write to [email protected]. Tell us your tales!
Femto Rationalization Falls Short
Thank you for publishing my letter, “Femto ‘Facts’—or Fake News?” along with the letter from Paul Ajamian, OD, in the October issue. FLACS is a major advance in cataract surgery and deserves a complete and open discussion. Thank you for beginning that.
However, I am almost amused by the editor’s response to my letter. Their defense for the inadequate references used to belittle FLACS in the Clinical Perspectives on Patient Care supplement is the authors’ “decades of hands-on expertise that also informed their views.” While it is true they have decades of experience, it has been in comprehensive optometry, including general exams, contact lenses, glaucoma treatment and so on. I wonder how that equates to the “decades of experience” of Dr. Ajamian, who helped found and establish comanagement of cataract surgery.
Dr. Ajamian has 40 years of experience being the lead optometrist in a surgical practice. Along the same lines, I have 36+ years of experience in a cataract and refractive surgery practice. It is our experience that tells us FLACS is a superior procedure in the hands of an experienced surgeon.
—Howell M. Findley, OD
Lexington, KY

