A recent study published in JAMA Ophthalmology provides updated estimates of the prevalence of glaucoma and its visual consequences using data from population-based studies, the National Health and Nutrition Examination Survey, medical claims and 2022 population estimates. The research team determined that Black adults in the US are approximately twice as likely as Caucasian individuals to have glaucoma and nearly three times as likely to have visual impairment, after adjusting for age and sex. The prevalence of both glaucoma and visual compromise arising from it also both increased substantially with age.1
 |
|
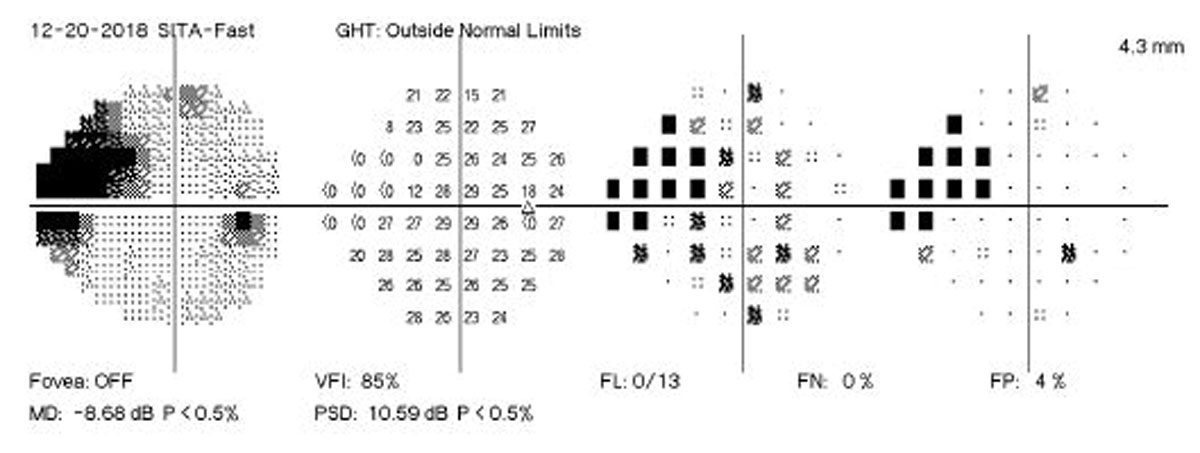
Prevalence estimates at the state and county level, as done with glaucoma in this study, can help guide public health planning. Photo: Brian Fisher, OD. Click image to enlarge. |
This meta-analysis used a variety of sources, some with prevalence data dating back to 1985. The study estimated that, as of 2022, 4.22 million people in the US (1.62% of adults) had glaucoma and roughly 35% of these individuals experience visual deficits as a result.
Substantial demographic and geographic disparities in glaucoma burden were also found. There was a prevalence of 1.62% among people aged 18 or older and 2.56% among those ages 40 or older. An estimated 1.49 million people were living with vision-affecting glaucoma, with a prevalence of 0.57% among people ages 18 or older and 0.91% among people ages 40 or older. The prevalence of glaucoma among people 18 years or older ranged from 1.11% in Utah to 1.95% in Mississippi. Black adults had a prevalence of 3.15% compared with 1.42% among white individuals; adults in the Hispanic and all other racial and ethnic categories combined had a prevalence of 1.56%.
“Such estimates can provide insights into the magnitude of the condition, enable forecasting of future trends and support appropriate allocation of health care resources,” the study authors wrote in their paper. “State- and county-level estimates that highlight variation in the prevalence of both glaucoma and vision-affecting glaucoma also allow for more tailored public health interventions.”1
A commentary also published in JAMA Ophthalmology noted that the study lacked sufficient representative data on older individuals (≥80 years of age) and racial and ethnic minority groups in the US (particularly Native American and Asian).2
“Due to the lack of data on American Indian and Asian individuals in the current study, the study has applied the prevalence estimates for Hispanic individuals to these groups,” the commentary noted. “It is important to note these individuals are disproportionately affected by primary angle-closure glaucoma, which confers a much higher risk of blindness than open-angle glaucoma, and, thus, the estimates of the prevalence of glaucoma and vision-impairing glaucoma may be substantially underestimated,” the commentary authors added.
The commentary concluded that expanding the research agenda on vision health in the US to include individuals in rural areas, older individuals and racial and ethnic minority groups is essential for achieving a better understanding of the burden of glaucoma in the increasingly diverse US population.2
| Click here for journal source. |
1. Ehrlich JR, Burke-Conte Z, Wittenborn JS, et al. Prevalence of glaucoma among US adults in 2022. JAMA Ophthalmol. October 17, 2024. [Epub ahead of print]. 2. Varma R, Jiang X. Glaucoma in the US—gaps in data on racial and ethnic minority and aging populations. JAMA Ophthalmol. October 17, 2024. [Epub ahead of print]. |

