 |
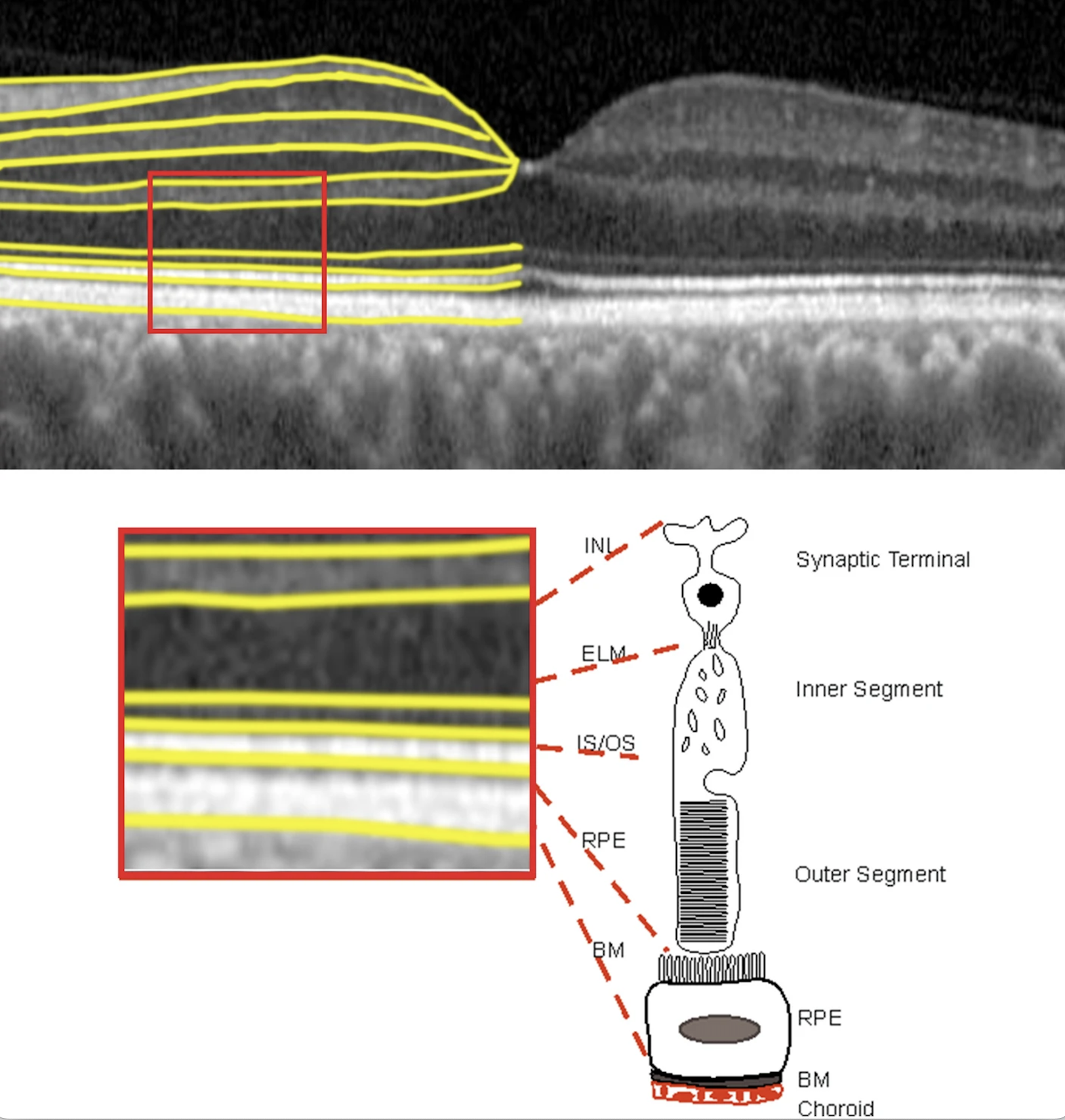
A new study in American Journal of Ophthalmology reveals a surprising and significant link between outer retinal thickness and brain health in patients with normal retinal aging, as well as early and intermediate AMD. Patients found to have thinner outer retina had considerably smaller hippocampus, lower occipital cortex regions of interest thickness, and lower cortical thickness in brain regions involved in Alzheimer’s disease and related dementias. Researchers say retinal imaging could serve a valuable and complementary role in understanding cognitive decline. Photo: Kaye RA, et al. Sci Rep 11, 23255 (2021). Click image to enlarge. |
The incidence of Alzheimer’s disease continues to grow exponentially, with some estimating it will affect more than 78 million people worldwide by 2030. However, imaging studies of brain aging have mostly been limited to neuroimaging, specifically MRI. Due to the cost associated with MRI, researchers have recognized retinal imaging to be a powerful, non-invasive and inexpensive way to study the brain via the eye. A new study in American Journal of Ophthalmology investigated how the outer retina in those with age-related macular degeneration (AMD) would correlate with brain changes associated with Alzheimer’s. The findings, which surprised the study authors themselves, reveal that a thinner outer retina was associated with the brain regions involved in memory.
Participants with thinner outer retina had significantly smaller hippocampus (β=0.019), lower occipital cortex regions of interest thickness (β=5.68), and lower cortical thickness in Alzheimer’s disease and related dementias (β=7.72). Significantly lower occipital cortex regions of interest (β=3.19) and dementia-related brain region (β=3.94) thickness was associated with participants with thinner total retina.
In AMD, the outer retina is impacted significantly and early, but little is known about its association with cognition or changes in brain morphometry. The authors noted the novelty of their study as it included patients with early or intermediate AMD, as well as those with normal retinal aging. “Limited literature exists on associations between neuroimaging and retinal imaging in older adults, particularly those with retinal diseases, such as AMD,” they wrote. “As retinal diseases are highly prevalent in aging populations, studies that include people with retinal disease are critical for understanding aging eyes and brain connections. In addition, several epidemiologic studies have shown that many retinal diseases are associated with higher risks of developing ADRD.”
The final cohort included 60 subjects (22 normal, 19 early AMD and 19 intermediate AMD) aged 70 to 87 (73% women). Seven participants were Black and the remainder were Caucasian, based on self-report. Linear regression was used to evaluate associations between retinal layer thickness measures (combined and averaged over central, inner, and outer ring) and dementia-related brain regions. MRI measurements included: total brain, cortex, cerebral white matter, gray matter and hippocampus volume, as well as occipital cortex thickness and cortical thickness in ADRD-related brain regions.
In this study, thinner outer retinal thickness in the outer ETDRS ring was the most frequently reported variable that predicted lower brain measurements, and most associated with atrophy of the brain regions involved in vision, memory and dementia-related regions. Thinner outer retina was associated with thinning of occipital regions of interest, lower hippocampal volume and brain regions known to show early structural and functional changes in dementia.
The association of outer retinal thinning with brain regions vulnerable to dementia and areas primarily involved in memory “was somewhat surprising,” the authors wrote in their paper. “It is possible that this association is unique to participants with normal macular aging and early and intermediate AMD. We recently published that in this cohort, outer retinal thickness was the only retinal layer that was significantly associated with cognition in this group.”
The authors point out that this pilot study, which had a small sample size, was meant to explore various relationships between retinal and brain health in people with early and intermediate AMD who are also at risk of developing age-related dementia. This “was not meant to study causal mechanisms,” they wrote. “Our study was not designed to investigate AD or any dementia specifically, and we used neuroimaging and cognitive proxy indicators of general brain health related to dementia. Thus, the generalizability of our results and hypothesized potential mechanisms should be interpreted with caution.
“Despite these limitations, the primary aim of our study was to identify associations and to highlight the predictive value of retinal layer thickness for brain atrophy, rather than to determine the exact magnitude of the associations,” the authors continued in their AJO paper. “Future research with larger sample sizes and independent replication studies will be crucial to confirm these associations, in which we also suggest exploring other retinal layer thickness variables that are highly correlated with the 'marker' identified in this study.”
In conclusion, the study suggests that retinal imaging, particularly outer retinal thickness, could be a complementary tool in evaluating risks of cognitive decline in individuals with normal retina aging, as well as early and intermediate AMD, but the authors say that “further research is warranted to determine whether these findings are specific to the AMD population or could generalize to populations with retinal diseases.”
| Click here for journal source. |
Jiang, Yu et al. Outer retinal thinning is associated with brain atrophy in early age-related macular degeneration. American Journal of Ophthalmology. Oct. 3, 2024. [Epub ahead of print.] |

