 |
| Prescribing a one-year course of valacyclovir to patients with HZO may help mitigate complications associated with the infection, as well as reduce the incidence of flare-ups that contribute to the development of chronic diseases like glaucoma. Dr. Cohen presented data supporting such an approach last weekend in Chicago at the Academy of Ophthalmology annual meeting. Click image to enlarge. |
Annually, more than one million people in the United States are diagnosed with shingles. Roughly 8% of these patients develop herpes zoster ophthalmicus (HZO) resulting from the impact of the virus on nerve pathways in the eye and forehead, causing significant unilateral pain, redness and impaired vision. While current treatment protocols consist of a seven- to 10-day course of antivirals, new research presented last week at the American Academy of Ophthalmology's annual meeting in Chicago found that extending the treatment duration to 12 months can significantly reduce the risk of ocular inflammation and infection in patients with HZO.
The study was led by Elisabeth J. Cohen, MD, whose career as a cornea surgeon was cut short over a decade ago after she contracted HZO and experienced significant vision loss. Feeling motivated to help find a solution for patients like herself, Dr. Cohen launched an eight-year research effort at NYU Langone Health medical center known as the Zoster Eye Disease Study (ZEDS), which investigated whether one year of treatment with a low dose of the antiviral drug valacyclovir could help reduce pain, ocular complications and disease flare-ups.
The study enrolled 527 participants across 95 medical centers in the US, Canada and New Zealand. Patients were randomized to receive a one-year course of either 1,000mg of valacyclovir (Valtrex) or a placebo. To be included in the study, participants had to be older than 18 and have a functioning immune system and kidneys, history of a typical HZO rash and active keratitis or iritis within the year before enrollment.
The results demonstrated a 26% reduction in the risk of new or worsening eye conditions (keratitis or iritis) at 18 months and a significant decrease in the number of flare-ups compared to those who received a placebo (30% reduction at 12 months and 28% at 18 months). The latter finding is particularly important for long-term outcomes, as “multiple flare-ups is what goes on to chronic disease and loss of vision,” Dr. Cohen pointed out in a recent interview for NYU Langone Health.
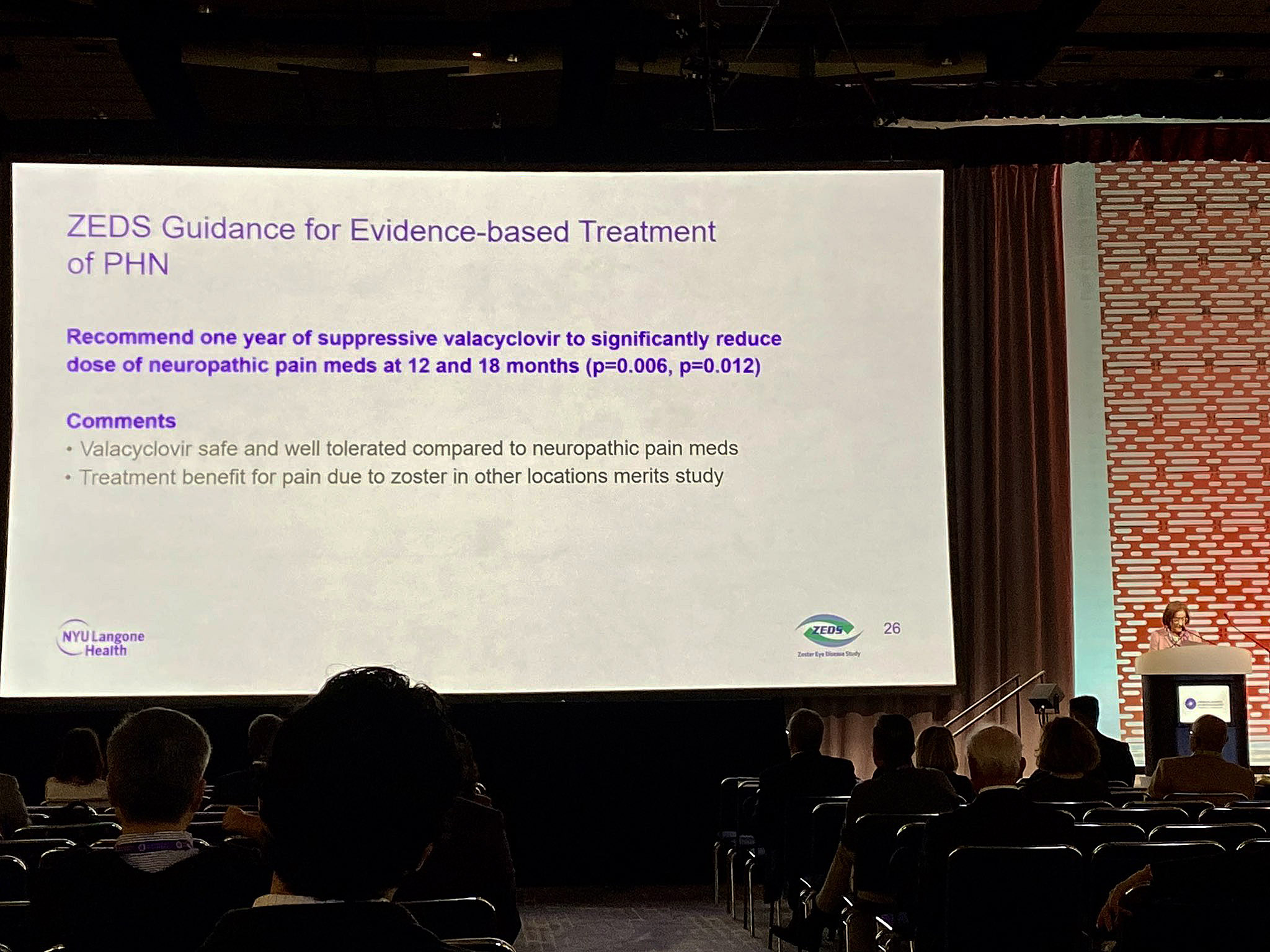
Also at 18 months, the study revealed that those on valacyclovir experienced shorter pain durations and reduced need for neuropathic pain medications. This was a prominent goal of the research, given that many pain meds have limited efficacy and can cause side effects such as dizziness in older patients.
“Our results support changes in clinical practice, with suppressive valacyclovir recommended to reduce new, worsening and repeated episodes of eye disease, as well as the need for neuropathic pain medication in HZO patients and in those with shingles-related pain,” Dr. Cohen concluded in a recent NYU Langone Health press release.
While these findings highlight the effectiveness and necessity of the new treatment regimen, Dr. Cohen and her fellow study investigators emphasize the critical role of prevention strategies in addressing the rising incidence of shingles among individuals over 50. Since the Shingrix vaccine is both widely available and effective, they argue that promoting vaccination within this older demographic could be advantageous.

