 |
Q:
I frequently have patients who are on Flomax (tamsulosin, Boehringer Ingelheim), have diabetes or are darkly pigmented and don’t dilate well. I am frustrated with my inability to get out to the periphery with binocular indirect ophthalmoscopy (BIO) and to scleral depress when necessary. Any suggestions?
A:
Not all clinical exams or patients are the same, so we can’t expect to be able to use all of the same tools with every patient, according to Jeffry Gerson, OD, of Grin Eye Care in Leawood, KS. “My standard lens for use with my BIO is a 20D, but I often use a 30D lens as needed,” Dr. Gerson says.
With a 30D lens, the field-of-view is wider, and it is often easier to get a good view into a smaller pupil. This is becoming increasingly more important with poor dilators, either from diabetes, Flomax use or other issues. The larger field (60 degrees vs. 75 degrees) can give better perspective, with the trade-off being a lesser degree of magnification (3.13x vs. 2.15x). A little practice goes a long way when dealing with this magnification issue, according to Dr. Gerson.
“The 30D allows for the shortest working distance with the greatest field-of-view,” Dr. Gerson says. Another advantage is that the 30D has a smaller diameter lens, which allows for easier manipulation for a doctor with smaller hands or when dealing with a patient with deeper inset or smaller eyes. The 30D is also ideal for kids who are not the most cooperative.
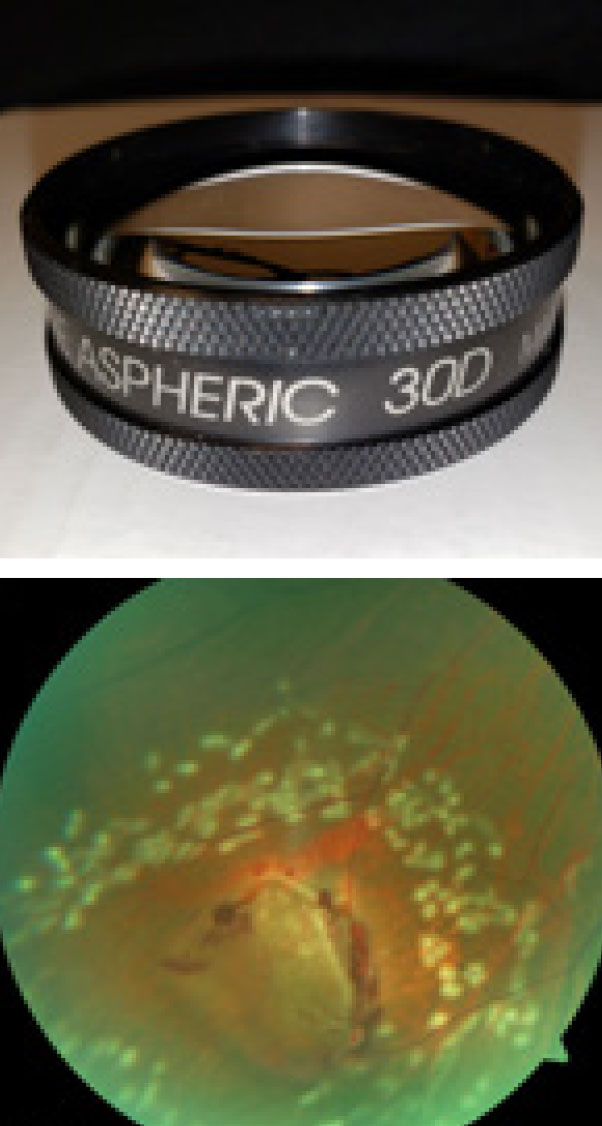 |
| Using a 30D lens can get you into a smaller pupil and out to the ora serrata. Photo: Omni Eye Services of Atlanta. Click image to enlarge. |
Scleral Depression
Besides the lenses used, Dr. Gerson recommends other techniques that can be helpful for a successful peripheral retinal examination, such as proper choice of dilating drops. Dr. Gerson uses a combination of 1% tropicamide and 2.5% phenylephrine for maximum dilation. “If one set doesn’t do it, instill another,” he states. “If possible, I always recline my patients, which helps get better views in the periphery,” Dr. Gerson says. A better view of the ora serrata means that scleral depression will be easier to perform.
“The lack of confidence some have with scleral depression stems from lack of practice or fear of hurting the patient,” he says. Dr. Gerson believes that each of these factors contributes to the other. “With some practice and a 30D lens, scleral depression becomes easier and more comfortable for patients,” he adds. Start with a long cotton swab, and graduate to a metal depressor if you need to. The more you do it, the more second nature it will become.
Scleral depression provides a dynamic view of the retina, which is critical when searching for retinal breaks in patients with symptoms like flashes and floaters. “Before one diagnoses a benign posterior vitreous detachment, one must rule out peripheral breaks, and that calls for scleral depression,” Dr. Gerson says.
Imaging and Dilation
Traditional fundus cameras only capture approximately 45 degrees. Ultra-widefield imaging is defined as a single capture that includes the far periphery of the retina in all four quadrants. This is a good screening tool that tips you off as to when and where to take a closer look with BIO and 30D.
If the image is normal but the symptoms tell a different story, protect yourself and your patient by dilating and taking a closer look. The most thorough retinal exam is probably a combination of the two modalities. Don’t give your patients the message that dilation is bad and ultra-widefield is good. “Clinically, I want to use every tool at my disposal,” Dr. Gerson says.

