 |
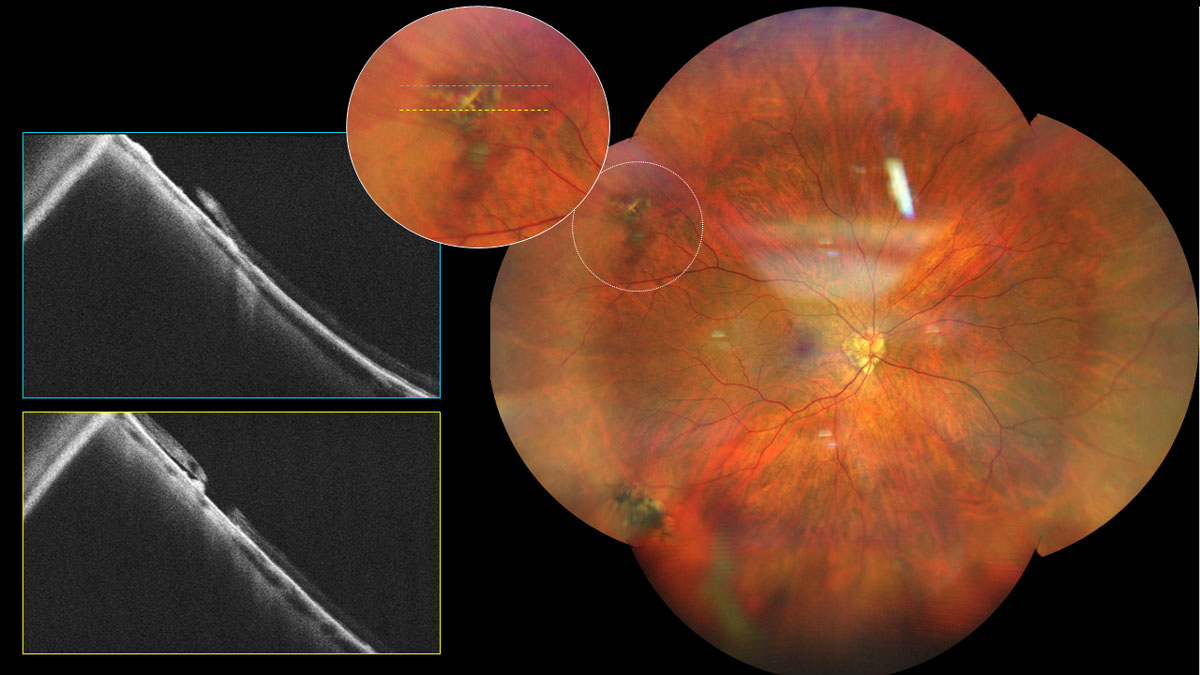
| A cross-sectional study showed that in longer eyes, failing to correct for ocular magnification leads to perceived narrowing of retinal vessels, while incorrect assumptions about telecentricity during magnification correction cause apparent vessel widening. This image is showing lattice degeneration in a high myope. Photo: Alia Cappellani, OD. Click image to enlarge. |
A recent research effort indicates that failure to account for ocular magnification in myopic eyes leads to apparent narrowing of vessels in eyes with longer axial length, while incorrect expectations about telecentricity during magnification correction create an optical artifact that results in perceived vessel widening.
These findings, published in Ophthalmology Science, suggest that “myopic changes in retinal vessel calibre are optical (not biological) in nature. Proper correction of this effect to accurately derive dimensional measures is a crucial—yet often overlooked—methodological consideration in ‘oculomics’ research investigating retinal biomarkers of systemic conditions,” the study authors noted in their paper for the journal.
This cross-sectional study included 82 normal right eyes from healthy participants between the ages of 16 and 31 years. The main outcome measures were central retinal arteriolar and venular equivalents. Researchers used semi-automated software to derive central retinal arteriolar and venular equivalents (CRAE and CRVE) from color fundus photographs. In this analysis, they assessed the influence of axial length (independent variable) on CRAE and CRVE, controlling for age, sex and ethnicity, both before and after magnification correction using different formulas.
These formulas, the study authors explained, estimate magnification based on different ocular parameters. This included axial length only (Bennnett’s formula), refractive error only (Bengtsson’s formula) and refractive error combined with keratometry (Littmann’s formula). The researchers point out that relying on refractive error is less accurate than axial length. “We also examined the impact of treating the non-telecentric fundus camera used in this study as telecentric when applying these magnification correction formulae,” they noted in their paper.
Before applying magnification correction, an increase in axial length was linked to a reduction in both central retinal arteriolar and venular equivalents. However, after magnification correction, this relationship was no longer observed, regardless of the correction formula used.
When incorrectly assuming the fundus camera to be telecentric, a bias emerged, showing increasing magnification-corrected CRAE and CRVE with increasing axial length, with statistical significance for CRAE corrected using Bennett’s or Littmann’s formulas, and for CRVE corrected using Bennett’s formula.
While highlighting their key findings, the study authors noted that axial elongation causes apparent narrowing of arterioles and venules due to decreased ocular magnification. Correct magnification adjustment removes this perceived reduction in vessel caliber, whereas incorrect assumptions regarding the camera design, or telecentricity, during magnification correction result in apparent vascular widening.
“Our findings, therefore, suggest an optical rather than biological link between myopia and vessel calibre,” the investigators stated. “The optical influence of ocular biometry and camera design on dimensional measures is a crucial, yet often overlooked, methodological consideration in oculomics research investigating retinal biomarkers of systemic conditions.
“Future oculomics studies are recommended to consider magnification correction and verify whether telecentric (constant p) or non-telecentric (varying p) correction is appropriate,” they wrote in Ophthalmology Science.
| Click here for journal source. |
Yii F, Strang N, Moulson C, et al. The optical nature of myopic changes in retinal vessel calibre. Ophthalmology Science. October 10, 2024 [Epub ahead of print]. |

