 |
Q:
A patient presented as an emergency with a left ptosis. How do I sort through this case without panicking?
“The first thing I think about in an adult presenting with acquired ptosis is myasthenia gravis (MG),” says Dennis Mathews, OD, a board-certified glaucoma and neuro-optometry specialist at Eye Specialty Group in Memphis.
MG is an autoimmune disease characterized by transient to constant muscle weakness. It can present with ocular motility restrictions and lid ptosis only, or it can progress to systemic involvement. Pathophysiology involves the production of antibodies that block normal responses of muscles to acetylcholine. Muscle-specific kinase (MuSK) antibodies are also involved in its development.
“Ocular MG can mimic other neuropathies and myopathies,” says Dr. Mathews. It is important to rule out cranial nerve III, IV and VI palsies and internuclear ophthalmoplegia.
 |
|
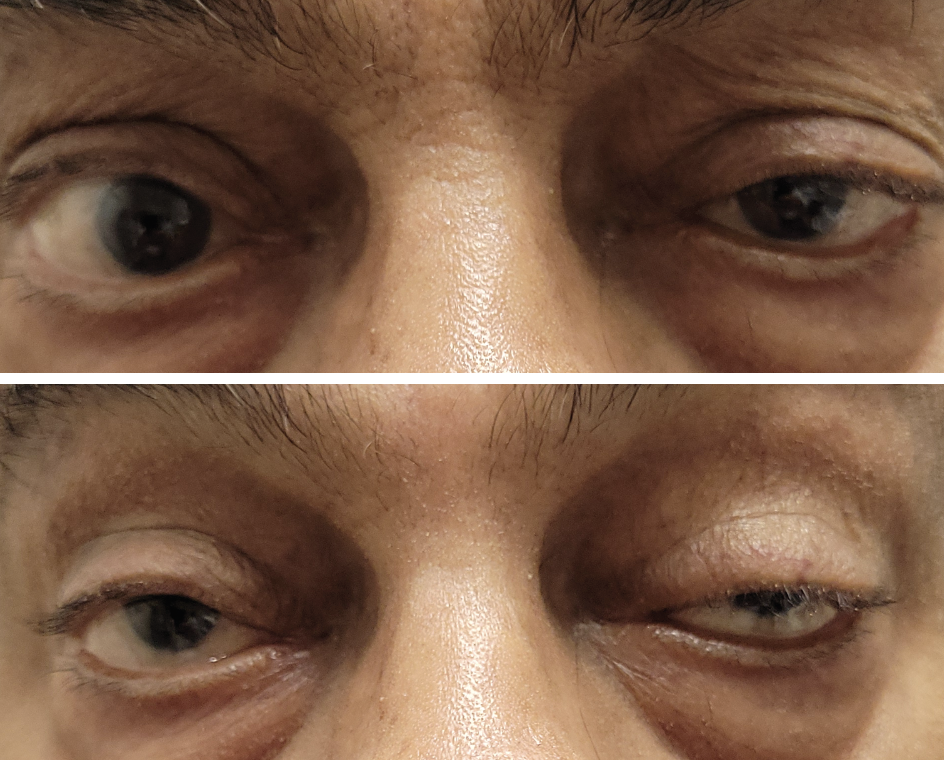
Sustained upgaze can help diagnose MG. Click image to enlarge. |
Testing 1, 2, 3
With myasthenia, the superior gaze stress test can help diagnose. Ask the patient to look up for a minute and watch the ptosis increase significantly from baseline. Other tests for MG include the ice pack test, looking for a 2mm or more increase in fissure size from baseline after two to five minutes. The tensilon test involves an IV injection of tensilon (edrophonium), looking for a resolution of the ptosis and oculomotor deficit within five minutes. This test does have risks and should be performed by a neurologist.
Laboratory tests such as acetylcholine blocking, modulating and binding antibody tests, along with MuSK antibody tests, can assist in diagnosis up to 80% of the time. In cases of a positive anti-acetylcholine receptor (anti-AchR) antibody test, thymoma should be ruled out with a chest CT scan.
According to Dr. Mathews, Horner’s syndrome should also be considered in any case of acquired ptosis, but it will often be accompanied by a miotic pupil. If a patient appears to have ocular MG but has lid retraction, extraocular muscle (EOM) restrictions and possible proptosis but not ptosis, rule out a thyroid condition.
A Flurry of Therapies
Past treatments were non-specific anti-inflammatories such as prednisone or immune modulators, including cyclosporine, azathioprine, methotrexate and tacrolimus. Mestinon (pyridostigmine, Bausch + Lomb) strengthens muscles by blocking the breakdown of acetylcholine.
Modern approaches use specific immune pathways to target a specific effect of this autoimmune disease. The first FDA-approved drug, Soliris (eculizumab, Alexion Pharmaceuticals), is a monoclonal antibody that blocks the complement inflammatory pathway, reducing damage to muscles and nerves.1 It is administered by IV infusion every week for four weeks. Only cases of MG that are AchR antibody positive are sensitive to this treatment. AstraZeneca’s Ultomiris (ravulizumab-cwvz) is a long-acting C5 complement inhibitor that works similarly but is longer lasting and dosed every eight weeks.2 Vyvgart Hytrulo (efgartigimod alfa/hyaluronidase, Argenx) is a subcutaneous injection also FDA-approved to treat MG in those who are anti-AChR antibody positive.3
Rystiggo (rozanolixizumab-noli, UCB) is an immunoglobulin monoclonal antibody that treats generalized MG patients who are acetylcholine antibody positive or MuSK antibody positive.4 Subcutaneous infusions are given every week for six weeks, then the treatment cycle is restarted, depending upon clinical response.
Zilbrysq (zilucoplan, UCB) is a complement inhibitor that blocks convertase, which cleaves C5.5 This is a peptide active with convertase. The patient administers prefilled syringes subcutaneously daily, much like insulin.
MG is an autoimmune disease that may commonly present with ocular signs and symptoms. It can mimic EOM palsies and throw the clinician off with the sudden ptosis. Appropriate testing and a calm, methodical assessment should lead to the correct diagnosis.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Thomas TC, Rollins SA, Rother RP, et al. Inhibition of complement acivity by humanized anti-C5 antibody and single-chain Fv. Mol Immunol. 1996;33(17-18):1389-401. 2. Vu T, Meisel A, Mantegazza R, et al. Terminal complement inhibitor ravulizumab in generalized myasthenia gravis. NEJM Evid. 2022;1(5):EVIDoa2100066. 3. Meisel A, Annane D, Vu T, et al; CHAMPION MG Study Group. Long-term efficacy and safety of ravulizumab in adults with anti-acetylcholine receptor antibody-positive generalized myasthenia gravis: results from the phase 3 CHAMPION MG open-label extension. J. Neurol. 2023;270(8):3862-75. 4. Bril V, Drużdż A, Grosskreutz J, et al.; MG0003 study team. Lancet Neurol. 2023;22(5);383-94. 5. Howard JF Jr, Bresch S, Genge A, et.al; RAISE Study Team. Safety and efficacy of zilucoplan in patients with generalised myasthenia gravis (RAISE): a randomised, double-blind, placebo-controlled, Phase III study. Lancet Neurol. 2023;22(5);395-406. |

