 |
|
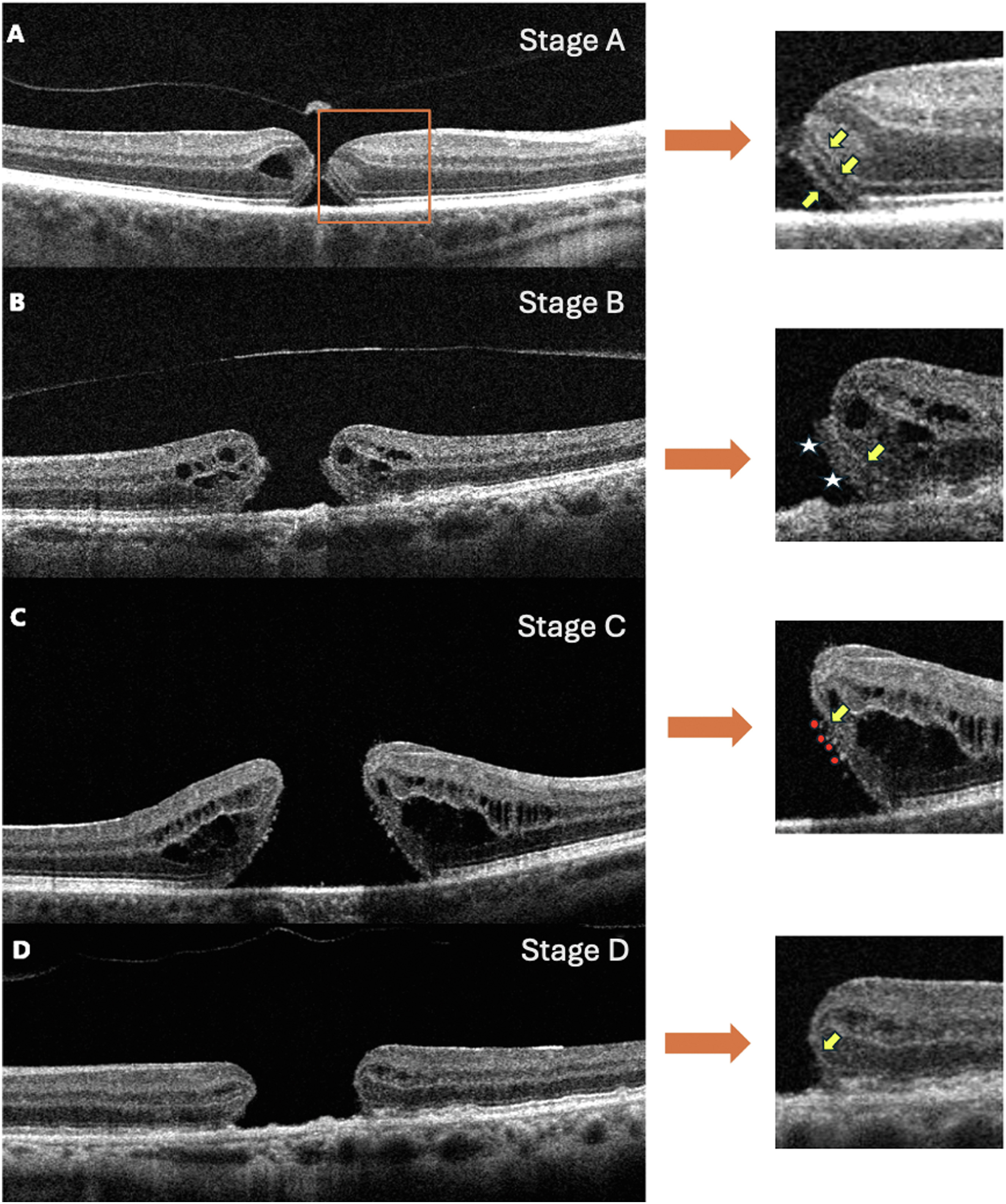
Researchers found that patients presenting with more advanced full-thickness macular hole at baseline had a longer duration of symptoms and worse VA at baseline and three months post-op. This image from the study shows the proposed staging on OCT: |
A recent observational study aimed to track and describe the sequential morphological changes of the outer retina after the development of a full-thickness macular hole (FTMH). This was done using a novel staging system based on spectral-domain OCT imaging, which the researchers proposed may serve as a novel biomarker with implications for modifying treatment and predicting outcomes.
The study reviewed the medical charts of 1,000 patients with idiopathic FTMH and focused its investigation on 52 individuals who had at least two preoperative SD-OCT scans (mean age: 65 years). This allowed researchers to review FTMH progression over time and assess the association between sequential outer retinal morphological changes on SD-OCT and baseline visual acuity, duration of symptoms and post-op functional outcomes.
In their paper on the study, published in Ophthalmology Retina, researchers described the following four distinct and reproducible stages they identified to characterize outer retinal morphologic changes at the FTMH borders:
- Stage A: separation of the neurosensory retina from the RPE with the well-defined external limiting membrane, ellipsoid zone and interdigitation zone (7.6% of eyes)
- Stage B: thickening of ellipsoid zone (51.9% of eyes)
- Stage C: patchy (moth-eaten) photoreceptor loss (30.7% of eyes)
- Stage D: severe or complete loss of inner and outer segments and/or bare external limiting membrane (9.6% of eyes)
“When assessing the preoperative OCT scans closest to the time of surgery, over a mean follow-up period of 288.9 days, 28.8% of eyes were in Stage B, 28.8% were in Stage C and 42.3 % were in Stage D,” the study authors reported.
Notably, the authors observed that patients at earlier stages at baseline demonstrated better postoperative visual outcomes than those at advanced stages. They noted that there was “a statistically significant association between increasing stage at baseline and longer duration of macular hole symptoms and worse visual acuity at baseline. Additionally,” they continued, “patients presenting with Stages B and C at the time point closest to surgery had better visual acuity outcomes three months postoperatively compared to those with Stage D.”
The staging system developed and used in this study displayed a direct correlation with the duration of macular hole symptoms and three-month outcomes of visual acuity, leading the researchers to conclude that “the extent of the outer retinal disruption is a crucial preoperative factor that predicts postoperative outcomes.” Elaborating on this, they noted that their data suggests “good anatomic recovery may be possible in eyes with an intact external limiting membrane; however, in eyes with large inner and outer segment defects, regeneration of the foveal floor may be difficult, resulting in a guarded prognosis for visual recovery.”
While there is currently no consensus on the optimal timing for surgery in FTMH, the study authors urge clinicians to thoroughly consider the status of the photoreceptors on presentation. “Despite the slow-paced progression of photoreceptor disruption at the FTMH border beyond Stage B, it is reasonable to advocate for early surgical intervention to maximize anatomic and functional outcomes,” they concluded.
| Click here for journal source. |
Pecaku A, Melo IM, Cao JA, et al. Morphologic stages of full-thickness macular hole on spectral domain optical coherence tomography. Ophthalmol Retina. October 24, 2024. [Epub ahead of print]. |

