 |
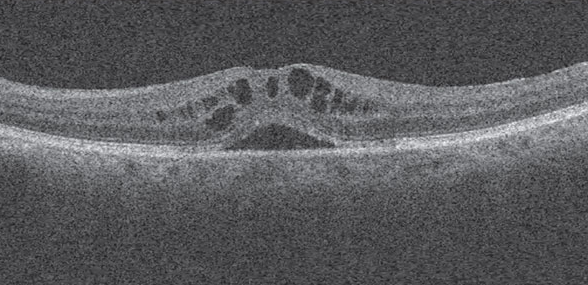
| New data from an IRIS Registry analysis suggests age, smoking, Medicaid insurance, non-white race and underlying retinal pathology contributes to poorer visual outcomes. Photo: Andrew S. Gurwood, OD. Click image to enlarge. |
A procedure without complications is never guaranteed. One common cause of decreased vision after cataract surgery is cystoid macular edema (CME). Recently, a retrospective, longitudinal study of IRIS Registry data was published in Ophthalmology, examining risk factors and visual outcomes of CME after cataract surgery. The study authors reported a low incidence of CME but emphasized a need to continue studying this common complication.
“There is a wide variation in the reported rates of CME after cataract surgery, depending on the study population and definition, and the general, practice-based incidence of clinical CME remains uncertain,” the authors explained in their paper. “This is where leveraging a large database such as the IRIS Registry can be helpful because it can provide insight into relatively rare conditions.”
The study looked at more than three million cataract surgeries in adults. Of those, 25,595 (0.8%) were diagnosed with CME, with a six-week average onset. The authors reported that patients with this complication were more likely to be male, under the age of 65, Black and have preexisting diabetic retinopathy. Additionally, CME patients were significantly more likely to have a poor visual outcome compared with patients without CME (VA 20/30 vs. 20/25 at 12 months).
The researchers also noted in their paper that smoking, Medicaid insurance, non-white race and baseline ocular comorbidities (e.g., macular degeneration and retinal vein occlusion) were associated with a poor visual outcome.
In the study, they pointed out that their 0.8% estimate is on the lower end of previous reports and corresponds to expected incidences of clinically significant CME. They wrote, “The true incidence of clinically significant CME is likely lower still because the limitations of the IRIS Registry database leave us unable to use a standard definition for CME.” Some of these limitations include a CME diagnosis given clinically or in order to justify use and reimbursement for confirmatory imaging.
“Patients who developed CME fared worse than patients who did not, with a mean final visual acuity of 20/32,” the authors concluded. “Older age, non-white race, smoking and retinal comorbidities compounded the risk of poor visual outcomes.” They suggested prophylaxis and close monitoring for those at high risk for postoperative CME.
Iftikhar M, Dun C, Schein OD, et al. Cystoid macular edema after cataract surgery in the United States: IRIS Registry (Intelligence Research in Sight) Analysis. Ophthalmology. 2023. [Epub ahead of print]. |

