 |  |
We are all too familiar with the constraints of the classic glaucoma treatment progression of drops-laser-surgery. Whether it is the cost of medications, compliance with administration of drugs or the need to tailor treatment to the stage of glaucoma, we routinely take a customized approach to this condition already. But there is an emerging, potentially disruptive treatment philosophy to consider: interventional glaucoma. It expands our arsenal of treatment options to further reduce the burden on our patients, allowing us to take earlier, more aggressive steps to treat glaucoma before it becomes uncontrollable.
In 2019, the interventional glaucoma philosophy received a major boost when the LiGHT trial outlined the benefits of selective laser trabeculoplasty (SLT) over topical meds as an initial treatment for glaucoma. This shift allows us to identify suboptimally controlled patients who are being treated with topical glaucoma medications and recommend reducing those agents in favor of early SLT, yielding improved ocular comfort and quality of vision, while also maintaining good glaucoma control.
 |
|
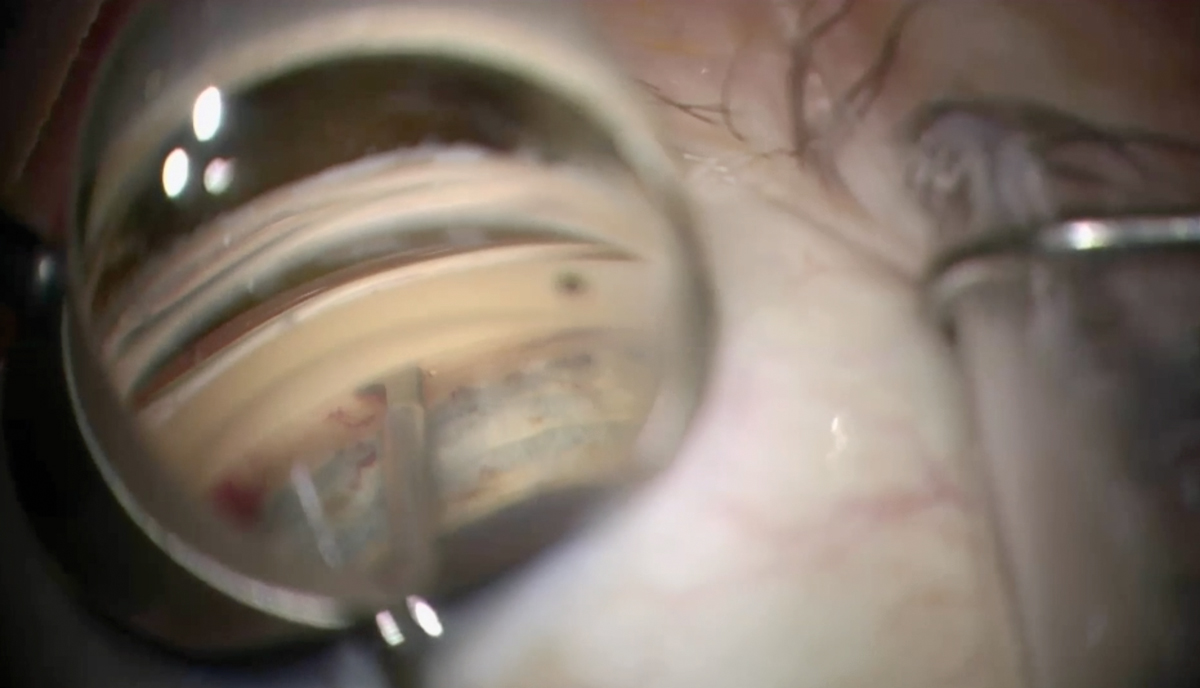
The Kahook Dual Blade excises a strip of trabecular meshwork to aid aqueous outflow. Photo: New World Medical. Click image to enlarge. |
The interventional glaucoma philosophy encourages a proactive approach and a more aggressive posture toward achieving IOP targets and disease control, relying on the numerous less invasive surgical options. We have become accustomed to thinking that minimally invasive glaucoma surgeries (MIGS) should occur at the time of cataract surgery; however, some experts are of the opinion that at least a few of these procedures could be considered as standalone treatment options as well in appropriately selected patients.
Candidates for Interventional Glaucoma ProceduresCataract Patients:
Pseudophakic Patients:
|
A few approaches are especially well-suited to consideration when adopting an interventional glaucoma mindset:
• Durysta. In 2020, Allergan received FDA approval for this agent—a biodegradable, intracameral bimatoprost implant that can be administered either at the slit lamp or in the operating room during the time of cataract surgery.
• Omni. This MIGS technique, from Sight Sciences, combines a canaloplasty with a trabeculotomy and can be performed with cataract surgery or in pseudophakic patients as an alternative to filtering surgery.
• Trabectome (Microsurgical Technology). This device creates a partial trabeculotomy, cauterizing and aspirating the nasal trabecular meshwork tissue roughly 90 to 180 degrees.
• Kahook Dual Blade (New World Medical). Similar to the Trabectome procedure, this method also removes tissue from the trabecular meshwork; however, it uses a dual-blade scalpel rather than cautery.
• Ab interno canaloplasty (iTrack, Ellex). Viscodilation of Schlemm’s canal is the method here, with the added advantage of breaking adhesions in the trabecular meshwork and irrigation of the collector channels.
We know that better IOP control in earlier stages of glaucoma decreases the risk of vision loss. Therefore, it is our responsibility to reach out to our ophthalmological colleagues and recommend less invasive, cost-saving and likely more efficient and effective treatment options for our patients.
Dr. Macintyre is an optometrist at Eye Care Associates of Nevada. He specializes in cataract surgery comanagement and perioperative care of cataract patients. He has no financial interests to disclose.
Dr. Zimmerman is an ocular disease resident at Dell Laser Consultants in Austin, TX. He has no financial disclosures.
Dr. Cunningham is the director of optometry at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose. Dr. Whitley is the director of professional relations and residency program supervisor at Virginia Eye Consultants in Norfolk, VA. He is a consultant for Alcon.

