 |
|
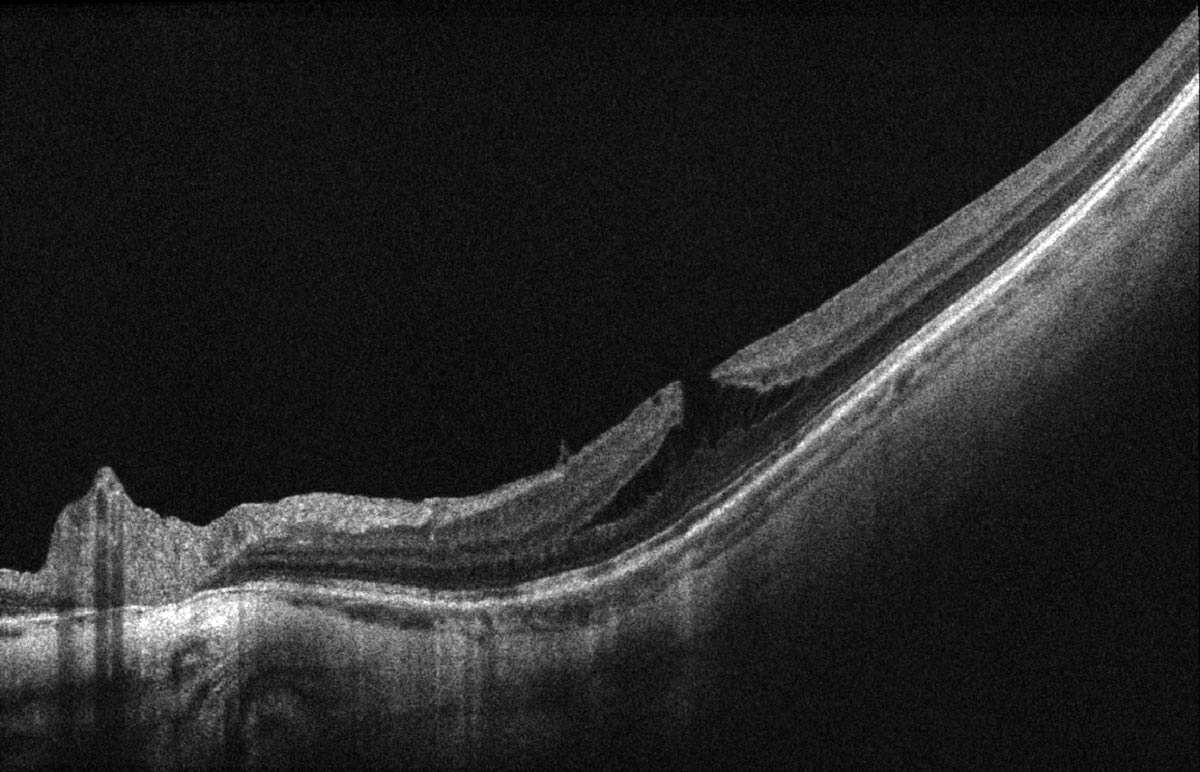
MTM with macular atrophy primarily manifests as maculoschisis with a lamellar macular hole; in this study, these were typically O-shaped, featured high outer retinal schisis and were thin-floored. Photo: Alia Cappellani, OD. Click image to enlarge. |
Myopic traction maculopathy (MTM) has emerged as a significant concern among patients with myopic macular atrophy, particularly in highly myopic eyes. A recent study aimed to elucidate the specific features of MTM in the context of macular atrophy, examining its evolution, surgical considerations, optimal procedures and overall outcomes.
A retrospective analysis was conducted on consecutive cases of highly myopic eyes with macular atrophy, classified as category 4 in the META-analysis for Pathologic Myopia study. The research included 87 eyes from 75 patients (19 men and 68 women).
Over a mean follow-up of 86 months, about half (50.6%) of macular atrophy cases showed various stages of MTM, primarily manifesting as maculoschisis with a lamellar macular hole (LMH; 81.8% of macular atrophy with MTM cases). These LMHs were typically O-shaped, featured high outer retinal schisis and had thin floors and a significant amount of thickened epiretinal tissue. Half of these cases either progressed to more severe maculoschisis (61%) or developed into macular holes with retinal detachment (39%); all of these patients required surgical intervention.
“MTM tends to progress,” the researchers wrote in their paper on the study, published recently in the journal Eye. “Macular hole in MTM is considered an unstable state that eventually leads to macular hole with retinal detachment.” Additionally, they noted, “The formation of an outer lamellar hole is an important intermediate stage in the development of macular hole with retinal detachment.”
The researchers also analyzed the outcomes of various surgical techniques used in cases of maculoschisis deterioration or macular hole with retinal detachment. They found that the inverted internal limiting membrane (ILM) flap technique, with or without fovea-sparing ILM peeling, was the most commonly employed surgical method (78%). Among these patients, most (94%) achieved structural stability postoperatively without secondary MTM, though the researchers noted that this procedure didn’t improve long-term vision.
“Since the inverted ILM flap technique effectively relieved traction with minimal complications or recurrences, we recommend surgical intervention when macular hole with retinal detachment or maculoschisis progression is observed,” they wrote in their paper.
Along with identifying a recommended treatment procedure, this study also serves to show that “macular atrophy contributes to the specific configuration and evolution of myopic traction maculopathy,” and “an O-shaped, thin-floored, lamellar macular hole with a high schisis is a characteristic feature,” the researchers concluded.
| Click here for journal source. |
Lee CY, Lai TT, Chen TC, et al. Myopic traction maculopathy in fovea-involved myopic chorioretinal atrophy. Eye. September 23, 2024. [Epub ahead of print]. |