 |
|
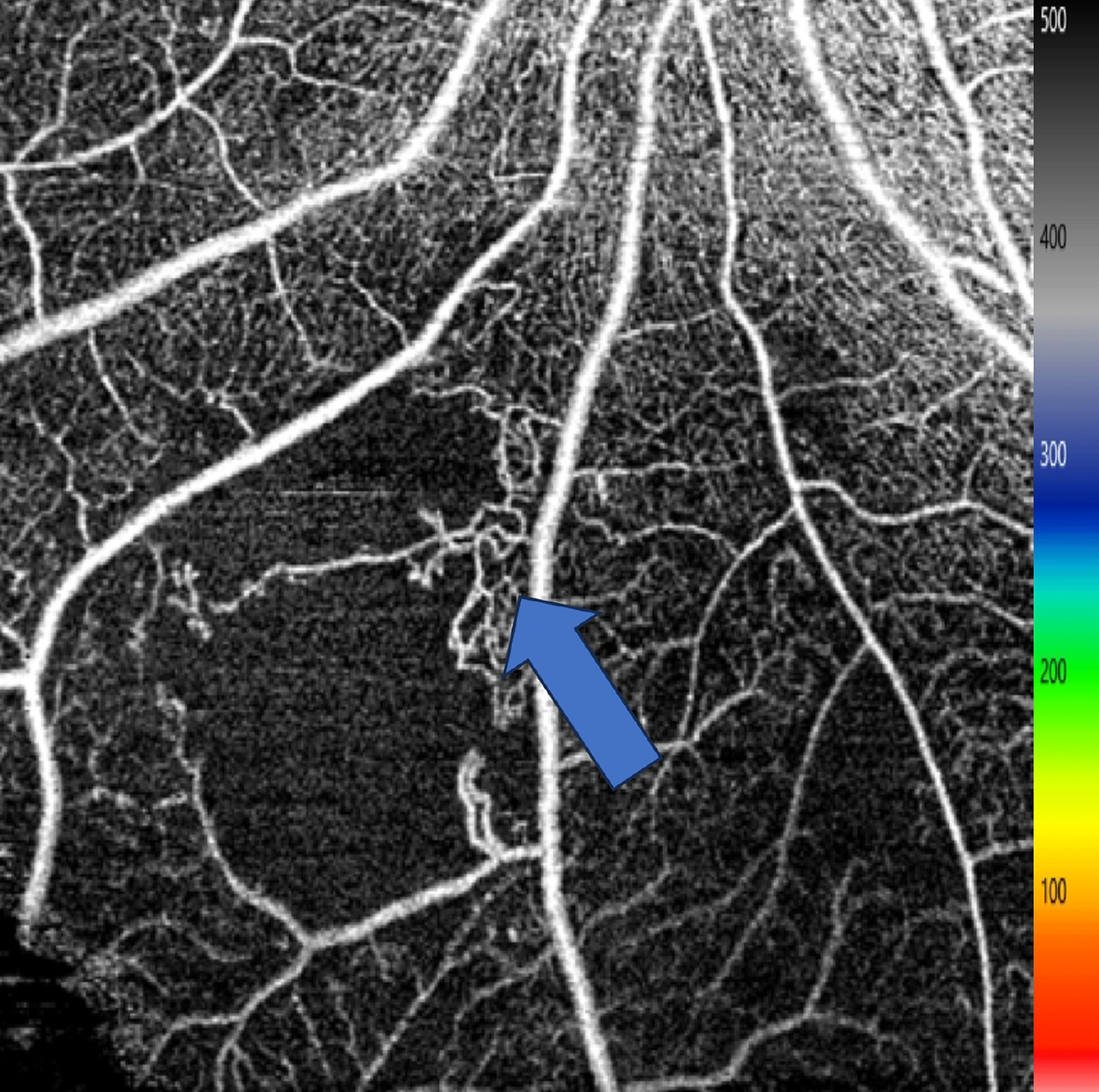
Greater attention to detecting and monitoring change in intraretinal microvascular abnormalities can aid the care of diabetic retinopathy patients. Photo: Jessica Haynes, OD. Click image to enlarge. |
OCT angiography (OCT-A) integrates vascular biomarkers with traditional structural factors to create a more personalized view of a patient’s status, potentially improving outcomes through timely and targeted intervention. In a recent study, Harvard researchers evaluated the utility of swept-source OCT-A imaging in predicting the occurrence of clinically significant outcomes in eyes with nonproliferative diabetic retinopathy (NPDR). They found eyes with intraretinal microvascular abnormalities (IRMAs) and ischemia are at a high-risk of developing significant clinical outcomes, including progressions to progression to proliferative DR (PDR). The team’s paper on the work was recently published in American Journal of Ophthalmology.
A total of 88 eyes with NPDR from 57 participants with at least two consecutive OCT-A scans over six-month follow-up period were included. The presence of IRMAs at baseline and the stability of these findings during follow-up period on 12x12mm angiograms were evaluated. Significant clinical outcomes were defined as occurrence of one or more of the following events at the last available clinical visit: significant DR progression (two-step DR progression or progression PDR; development of new center-involving diabetic macular edema (DME) and initiation of treatment with PRP or anti-VEGF injections during the follow-up period.
This study found that greater ischemia is a significant and independent risk factor for disease progression, which aligns with prior research. “In fact, previous studies have shown that the presence of extensive areas of capillary nonperfusion, defined as over 70% of the area in the entire retinal image on fluorescein angiography, is a critical indicator of advanced DR and often indicates a poor visual prognosis,” the authors explained in their AJO paper. “Patients with active PDR were found to have a significantly larger area of peripheral capillary nonperfusion six months following PRP treatment.” Although midperipheral nonperfusion has previously been linked with worsening of diabetic retinopathy, the authors note that ischemia at the posterior pole may be more indicative of future disease progression.
“This research underscores the importance of our findings,” they wrote, and proposed the use of widefield OCT-A as a noninvasive and reproducible alternative to fluorescein angiography for anticipating DR outcomes.
A previous study by the same authors showed that OCT-A is superior to color photos in detecting IRMAs, thus making the case that OCT-A significantly enhances the detection of this subtle finding. The study also showed that nonstable IRMAs during follow-up were strongly associated with both significant DR progression and significant clinical outcomes as an independent risk factor, the team explained in their paper.
What the authors found interesting is that despite IRMAs occurring more frequently with increasing DR severity at baseline, no correlation was found between the presence of IRMAs and DR progression or outcomes. “A possible explanation is that IRMAs exhibit various subtypes, each potentially leading to differing levels of stability and progression risk,” they wrote. “Our findings emphasize the importance of continuous monitoring of IRMA changes, as it provides dynamic insights into the progression of DR that might be missed by single time point evaluations.”
| Click here for journal source. |
Ding X, Romano F, Garg I, et al. Expanded field OCT angiography biomarkers for predicting clinically significant outcomes in non-proliferative diabetic retinopathy. Am J Ophthalmol. October 15, 2024. [Epub ahead of print.] |