 |
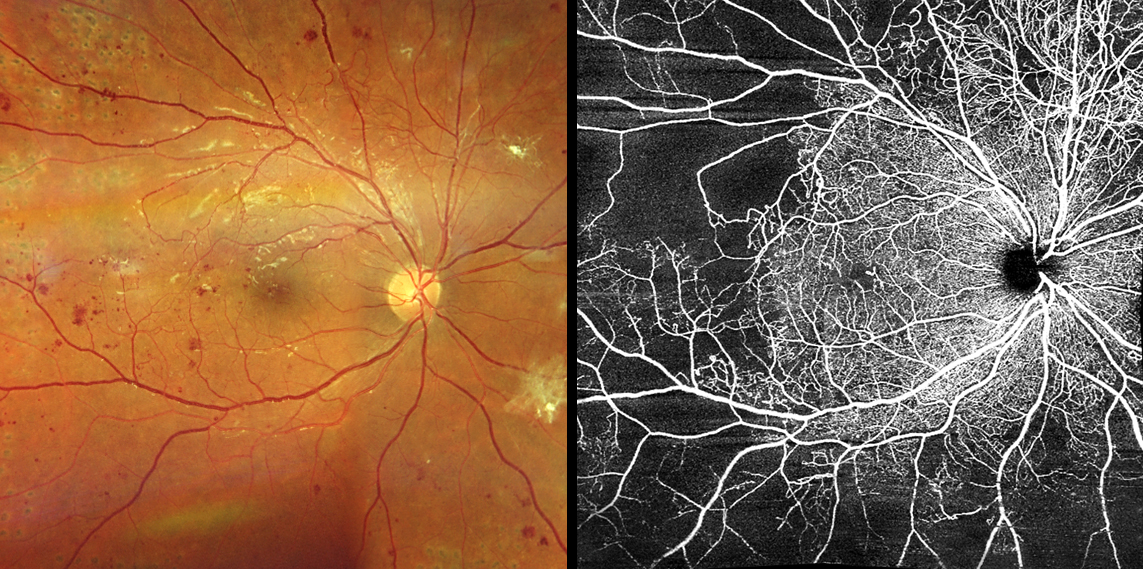
Previous investigations have found disruptions to circadian rhythm like shift work and social jetlag are associated with type 2 diabetes, and glucose homeostasis is essential in maintenance of normal physiological function of retinal cells. Photo: Carolyn Majcher, OD. Click image to enlarge. |
The disruption of the bodily clock, or circadian rhythm, has been reported to aggravate progression of diabetic retinopathy (DR). Used as a method in measuring individual circadian time and influencing behavior, a variable called rest-activity rhythm (RAR) was analyzed in a new study in relation with DR risk.
Included in the investigation were 1,096 diabetic patients aged 40 or older from the 2011 to 2014 National Health and Nutrition Examination Survey. RAR metrics were generated from data collected via a wearable sleep monitor, including measures of interdaily stability (IS), intradaily variability (IV), most active 10-hour period (M10), least active five-hour period (L5) and relative amplitude (RA).
Researchers used a wearable sleep monitor to gather information, which helped them analyze patterns like how consistent daily activities were (interday stability), how much activity varied within a day (intraday variability), the most active 10-hour period, the least active five-hour period, and the overall activity rhythm.
Of all participants, DR prevalence was 20.5% and mean age of participants was 62.3, with 49.6% being male. After considering other factors, it was found that greater daily activity variation was linked to a higher chance of having DR. Specifically, those with the highest variation had a 136% higher risk compared to those with the lowest variation. On the other hand, being more active during an individual’s most active 10-hour period was linked to a lower risk of DR, with those in the highest activity group having a 48.8% lower risk. Additionally, the study identified three distinct groups of individuals linked with greater or lesser risk of DR. Those with high variation and low activity had a higher risk compared to those with the opposite findings (low variation, high activity).
Essentially, the authors explain that these results indicate a more fragmented rhythm and lower peak activity level may be associated with increased DR risk. Generally, the explain that “these findings highlight the potential advantages of maintaining a regular sleep-activity rhythm and having high activity levels during the daytime in terms of delaying the onset of DR.”
With increasing physical activity level, DR progression alleviates to a degree, and some studies even demonstrated higher physical activity is independently associated with lower DR incidence. Being active may improve glycemic control and vitamin D levels, the latter of which has been reported to possibly inhibit retinal inflammation and retinal neovascularization. Hence, the authors speculate that subjects with high activity pattern may have batter glycemic control and higher levels of vitamin D, “thereby ameliorating DR-related pathogenesis.”
Subjects with high intraday variation—the group with 136% higher risk of DR—showed a less stable or more fragmented rest-activity pattern, with frequent transitions between activity and rest, typically resulting from irregular sleep patterns, inconsistent wake times or frequent naps. Melatonin is the primary hormone involved in sleep-wake cycle regulation and is, with deficiency, known to be responsible for sleep disorders. The hormone exhibits protective effects potentially beneficial to DR patients, including anti-oxidative, inti-inflammatory and anti-apoplectic properties. Consequently, this has the researchers speculating “that some participants, due to a lack of melatonin, may lose its protective effect on the retina and become more prone to developing DR.”
| Click here for journal source. |
Wang Z, Wu M, Li H, Zheng B. Association between rest-activity rhythm and diabetic retinopathy among US middle-age and older diabetic adults. Front Endocrinol (Lausanne). September 16, 2024;15:1440223. |

