 |
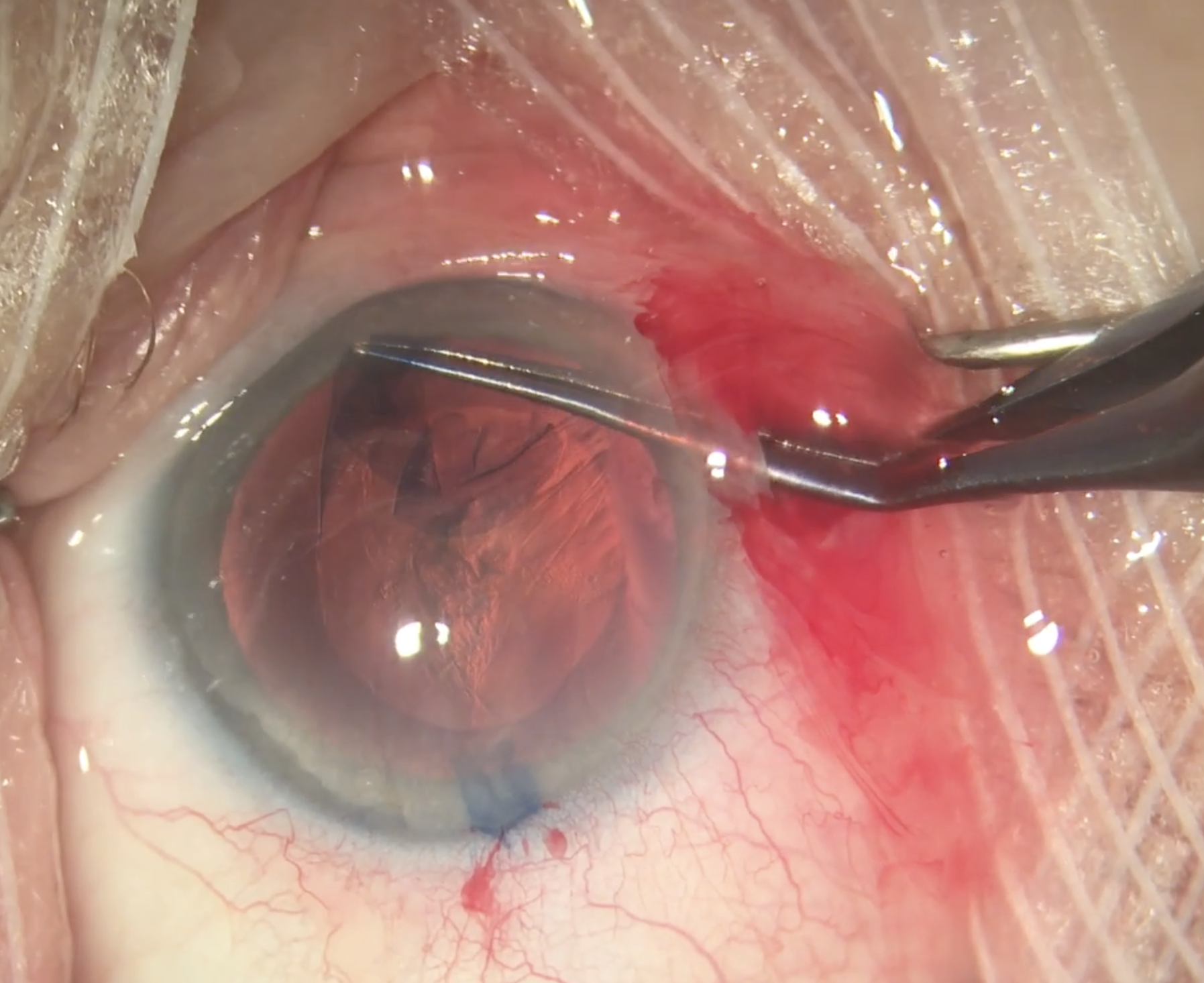
| A recent meta-analysis of 57 clinical trials published in the journal Vision suggests the optimal time to measure IOP after cataract surgery is between four to eight hours postop. Hours four, six and eight had an increase of IOP from baseline of +1.38, +0.83 and +0.93, respectively. With data from over 6,300 patients, the study highlights the risks of missing these spikes should IOP be measured too soon following surgery and offers clearer guidance for surgeons who may have otherwise monitored this data in an unstructured manner. Photo: Christina Tran, BS, and Leonid Skorin, Jr., DO, OD. Click image to enlarge. |
Recommendations on the optimal time to measure IOP following cataract surgery are vague, ranging from within the first 24 hours for high-risk patients, to 48 hours postop in low-risk patients. Without specific guidance, timing has become a matter of convenience for the surgeon, which could lead to missed IOP spikes if done too soon or too late. A considerable amount of research exists with data accounting for IOP measurements taken at different time points following uncomplicated cataract surgery, and a new study published in the journal Vision reports the results of a meta-analysis suggesting the best time to measure IOP may be within the first four to eight hours following surgery.
This study included 57 randomized clinical trials published between 1992 and 2023, from which they derived a total of 6,318 participants and 7,089 eyes. A total of 43.7% of participants were male, and the mean age of all subjects was 68.4. The most significant decrease in IOP from baseline was in postoperative hour one (-2.08), while hour two has a non-significant increase (+.081). Postop hours four, six and eight were the only timepoints to show a significant increase in IOP (+1.38, +0.83 and +0.93, respectively). There was no significant change in IOP on postop day one, and a non-significant decrease on day two (-0.36). Researchers conducting this meta-analysis therefore concluded that the data supports postop hours four to eight as the optimal IOP measuring timepoints to avoid missed IOP spikes.
The authors wrote in their paper that measuring IOP sooner than two hours may be misleading, “as IOPs were found to be lower than baseline, likely related to surgical techniques to manage wound closure following aspiration of OVD. The results indicated that a continuous decrease in IOP at the three-days, seven-days, and 30-days is expected and consistent with evidence that retained OVD is unlikely to be causative after two to three days.”
Peri-operative medications were also recorded and analyzed in this meta-analysis, of which there was a significant variability. The most common preop medications were either an antibiotic or an NSAID, and—for those that did report the administration of medications intraoperatively—the most common were found to be antibiotics, carbachol and/or a steroid. A combination of antibiotics, steroid and/or NSAID were used postoperatively in a majority of the studies.
“These medication combinations have been shown in some studies to have a small effect on IOP in the immediate days following cataract surgery,” the authors wrote. “Ten studies reported the use of an IOP-lowering medication, which included carbonic anhydrase inhibitors, beta-blockers, prostaglandin analogs, and alpha agonists. These medications were used either prophylactically to prevent IOP elevations, to lower IOP in patients who were actively experiencing a dangerous spike, or as routine treatment for glaucoma patients. Despite these medications having peak effects between two and eight hours post-administration, they did not seem to prevent the IOP spikes noted from four to eight hours later.”
Some limitations were noted by the authors, including the variability in the quality scoring of the included studies, which could risk bias assessment due to unclear blinding. “However, as the current literature only offered a small number of relevant publications, all were included, irrespective of their quality score,” they said. Asymmetrical funnel plots at various follow-up timepoints could also be a limitation, however, Egger’s regression test provided weak evidence for the presence of small-study effects. “Asymmetry could have been caused by several other reasons, including difficulty in the interpretation of the funnel plot for a small group of studies, high heterogeneity and small effect sizes,” continued the authors.
It’s also worth highlighting that none of the studies included in this meta-analysis mentioned patient position during IOP measurement. “This is important to note as clear corneal thickness, astigmatism and patient position can potentially affect IOP measurements,” they wrote.
In conclusion, this study provides more specific guidance for when IOP should be measured, with caution not to do so prior to the four-hour timepoint when spikes became significant. “Continuous practice assessment to determine factors that optimize patient-reported outcomes and experiences in the context of evidence-based quality care may be the key to best practice recommendations,” the authors concluded in Vision.
| Click here for journal source. |
Herspiegel WJ, Yu BE, Algodi HS, Malvankar-Mehta MS, Hutnik CML. Optimal timing for intraocular pressure measurement following phacoemulsification cataract surgery: A systematic review and a meta-analysis. Vision. November 8, 2024. [Epub ahead of print.] |

