|
As technology for retinal imaging improves, the very nature of the retinal exam continues to change. While the standard of care remains the dilated eye examination to assess retinal health, better image capture technology and even the advent of artificial and augmented intelligence are changing the way optometrists approach diagnostic testing for retinal conditions.
Out With the Old
New CPT codes for the manual retinal exam went into place in January 2020, which redefine the extended ophthalmoscopy codes. The old codes allowed for a new (92225) or subsequent (92226) examination and were unilateral in nature; the new CPT codes 92201 and 92202 are now specific to the area and method of examination:
• 92201: Ophthalmoscopy, extended, with retinal drawing and scleral depression of peripheral retinal disease (e.g., for retinal tear, retinal detachment, retinal tumor) with interpretation and report, unilateral or bilateral.
• 92202: Ophthalmoscopy, extended, with drawing of optic nerve or macula (e.g., for glaucoma, macular pathology, tumor) with interpretation and report, unilateral or bilateral.
Additionally, new technology can simultaneously capture a widefield or ultra-widefield image of the retina in color, image with autofluorescence and perform an OCT variant. Practitioners may be tempted to abandon the traditional manual retinal exam in favor of simply capturing a retinal image and making a clinical judgement from that—and therein lies a host of challenges.
A Medicolegal Challenge
Many may feel the image capture of an ultra-widefield image is less traumatic on a patient, is more convenient, takes less time and does a better job than they can do manually; however, this is not the current medicolegal standard. Manufacturer websites clearly state that the technology is complementary to the doctor’s examination and allows for additional diagnostic capabilities.
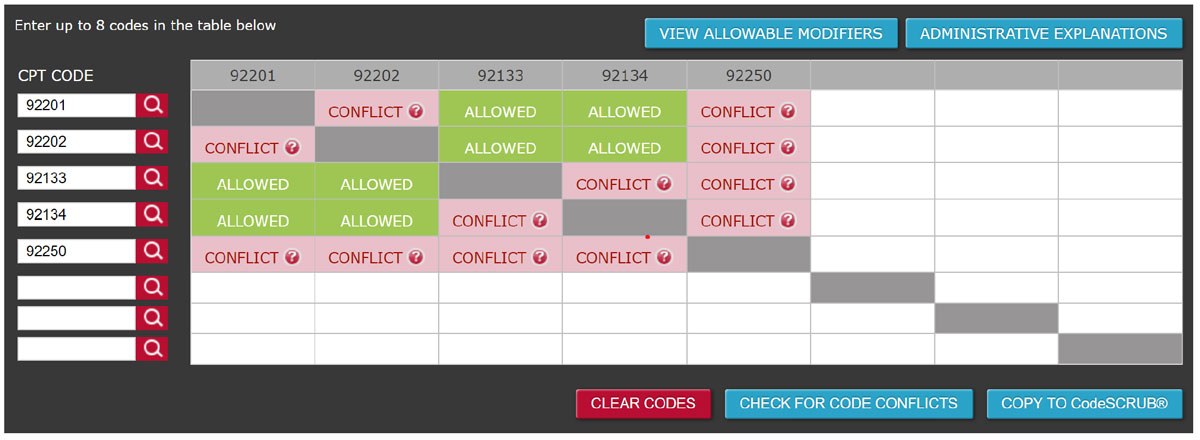 |
| Fig. 1. As this analysis by www.codesafeplus.com shows, myriad CCI conflicts exist when attempting to code for extended ophthalmoscopy on the same day as an OCT and fundus photography. Click image to enlarge. |
A Coding Challenge
The NCCI, or CCI, edits are a set of federal rules that stipulate what CPT codes can be coded for on the same date of service. These rules exist to preserve standards of care and to help with national coding consistency for specific disease states. Carriers follow these rules when they are approving or denying claim submissions.
When using devices that capture many images simultaneously, it is the clinician’s responsibility to determine which image is going to be used, coded for and billed for prior to capturing the image, because the CCI edits don’t allow for many of these procedures to be performed on the same date of service (Figure 1).
Yet I continually see practitioners not respecting these rules or using a modifier to get around them. Be forewarned: if you are going to violate a rule, your medical record should demonstrate that it was imperative, and you must follow the guidelines when using appropriate CPT modifiers to further define the clinical situation you were facing that forced you to violate a rule.
Also of note: none of these codes are approved for telehealth.
The CCI edits don’t always make sense because technology is quickly outpacing the coding rules, but they are the rules, for now. Understanding and respecting them is crucial for clinical practice.
Send your coding questions to [email protected].