 |
A 37-year-old Caucasian woman presented emergently after she noticed white spots on her corneas of one month’s duration. Her vision was unaffected, her eye was not red and she reported no discomfort. There was no history of trauma. Her systemic and ocular histories were unremarkable. She denied allergies of any kind.
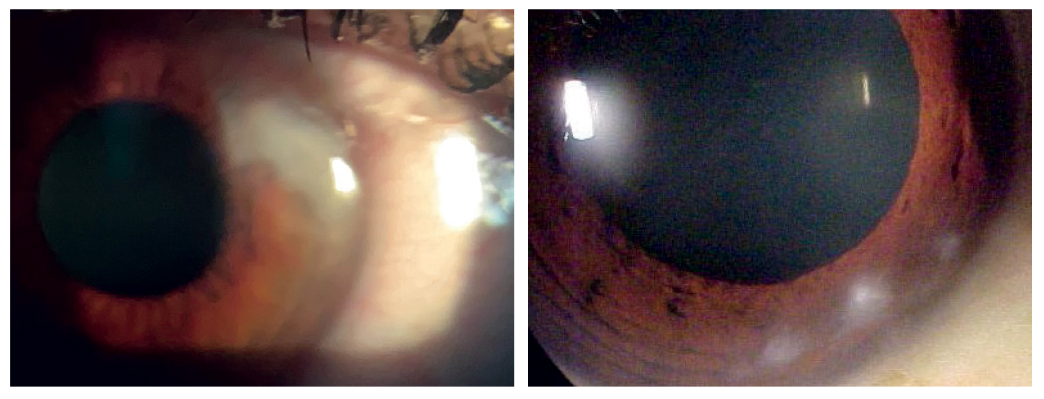
Her best-corrected entering visual acuities measured 20/20 OD, OS and OU at distance and near. Her external examination was normal and there was no afferent pupil defect. The pertinent anterior segment findings are demonstrated in the photographs. Goldmann applanation tonometry measured 15mm Hg OU. The dilated fundus findings were normal.
Additional studies included check of the corneal epithelium and conjunctivae with fluorescein stain to ensure intact tissues without evidence of chronic ocular surface disease. The tear prism, cilia and meibomian glands were evaluated for infectious or inflammatory meibomian gland dysfunction. The lids were everted to inspect for foreign bodies; none were found. Corneal sensitivity testing confirmed proper innervation. All layers of the cornea were inspected to document the location of the lesion, and the iris was evaluated to investigate any potential relation to anterior chamber angle dysgenesis syndromes. Photodocumentation was completed.
 |
|
Slit lamp presentation of each eye showing subepithelial deposits. Click image to enlarge. |
Salzmann’s Lesions
The diagnosis in this issue is giant Salzmann’s lesions OU. Salzmann’s nodular degeneration (SND) is characterized by one or multiple superficial blue-white nodules in the paracentral or midperipheral region of the cornea.1-7 The slowly progressive non-inflammatory process was first reported in 1925 by the Austrian ophthalmologist Maximilian Salzmann.5 He theorized it to be a corneal degeneration secondary to phlyctenular or trachomatous keratitis.5 SND is often bilateral but can be unilateral.1-5 It has a variable clinical presentation with one or more nodules producing no symptoms or having the capability of causing foreign body sensation and/or blurred vision depending upon their size and location.1-5
SND most commonly occurs in Caucasian women appearing in the fifth to eighth decades of life, but has been documented in younger persons.1,2,5 Risk factors include characteristics of ocular surface disease (e.g., tear dysfunction syndrome, meibomian gland dysfunction), chronic contact lens use and any systemic/adnexal condition than can affect tear production, integrity or volume (such as thyroid eye disease), corneal injury and ocular surgery.1,2,4,6,7
Histologically, Salzmann’s lesions are subepithelial nodules with thin overlying corneal epithelium. Eosinophilic material disrupts or replaces Bowman’s layer.1,2,8
SND pathogenesis is not fully understood but is thought to occur secondary to poor corneal epithelium protection, resulting in disruption of the epithelial-stromal interface, which allows penetration of epithelial-derived growth factors to invade into the stroma. This process produces subsequent activation of stromal fibroblasts and eventually leads to subepithelial deposition of disorganized extracellular membrane components.1,2,5,8
Workup and Management
The literature has documented some recommended diagnostic investigations, which include ultrasonic pachymetry, anterior segment OCT, ultrasound biomicroscopy and confocal microscopy.2,9
Most cases can be monitored without any intervention whatsoever. Some mildly symptomatic cases may respond well to topical lubrication, along with anti-allergy and anti-inflammatory therapies available to augment supportive treatment.1,5 Scleral contact lenses have been used to both sequester the cornea in a reservoir of tears and to provide it with a remediated environment as an alternative to more invasive surgical approaches.3
Surgical intervention is recommended for highly symptomatic individuals.1 Superficial keratectomy may be performed with or without intraoperative mitomycin C. Phototherapeutic keratectomy can be assisted with amniotic membrane support. While these procedures have been successful at removing lesions and reducing corneal irregularity, they have variable recurrence rates, up to 31% in one study.1 There are no cases in the literature demonstrating spontaneous resolution.5
The patient was educated about the condition and placed on lubrication therapy. She was referred to a cornea specialist, where the diagnosis was confirmed. She remains asymptomatic with excellent vision.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Paranjpe V, Galor A, Monsalve P, Dubovy SR, Karp CL. Salzmann nodular degeneration: prevalence, impact, and management strategies. Clin Ophthalmol. 2019;13(7):1305-1314. 2. Maharana PK, Sharma N, Das S, Agarwal T, Sen S, Prakash G, Vajpayee RB. Salzmann's Nodular Degeneration. Ocul Surf. 2016;14(1):20-30. 3. Chiu GB, Bach D, Theophanous C, Heur M. Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) scleral lens for Salzmann's nodular degeneration. Saudi J Ophthalmol. 2014;28(3):203-6. 4. Stem MS, Hood CT. Salzmann nodular degeneration associated with epithelial ingrowth after LASIK treated with superficial keratectomy. BMJ Case Rep. 2015;2015(1):bcr2014207776. 5. Brown AC, Nataneli N. Salzmanns Nodular Corneal Degeneration. 2020 Jul 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020: 32809519. 6. Yang MC, Al-Hashimi S, Rootman DB. Salzmann's nodular degeneration of cornea associated with thyroid eye disease. Orbit. 2019;38(4):325-327. 7. Hamada S, Darrad K, McDonnell PJ. Salzmann's nodular corneal degeneration (SNCD): clinical findings, risk factors, prognosis and the role of previous contact lens wear. Cont Lens Anterior Eye. 2011 Aug;34(4):173-8. 8. Stone DU, Astley RA, Shaver RP, Chodosh J. Histopathology of Salzmann nodular corneal degeneration. Cornea. 2008;27(2):148-51. 9. Hurmeric V, Yoo SH, Karp CL, Galor A, Vajzovic L, Wang J, Dubovy SR, Forster RK. In vivo morphologic characteristics of Salzmann nodular degeneration with ultra-high-resolution optical coherence tomography. Am J Ophthalmol. 2011;151(2):248-56.e2. |

