 |
|
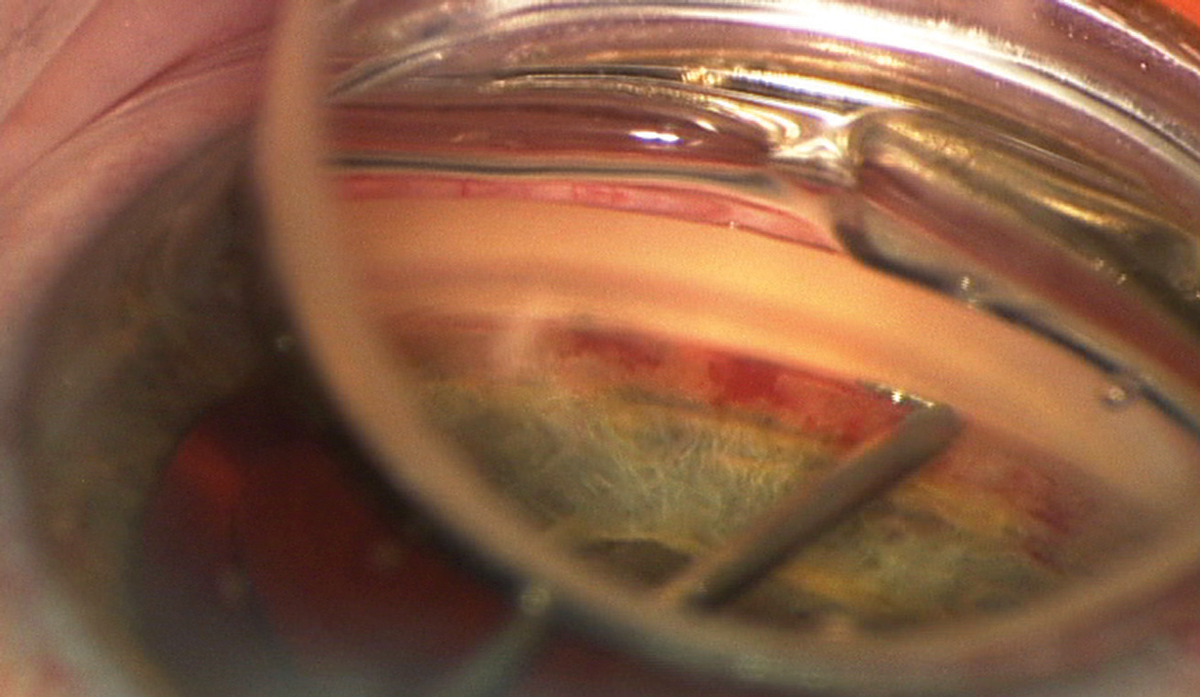
That distribution of glaucoma procedures (traditional vs. MIGS) among MDs in the United States was related to physician factors such as urban/rural setting and year of training. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
As newer glaucoma procedures become more prevalent, expanding the range of options, it is important to understand factors that influence the preferences and choices of subspecialists.
A recent study published in Journal of Glaucoma examined the relationship between glaucoma procedure distribution and physician characteristics such as urban/rural setting and duration of practice. Using data from the 2019 Centers for Medicare & Medicaid Services (CMS) Physician Payment and American Board of Ophthalmology databases, the research team found that providers who only perform MIGS procedures account for a significantly greater percentage of glaucoma procedures in non-metropolitan compared to metropolitan areas (78% vs. 50%). Also, ophthalmologists with more recent certification years performed a greater proportion of traditional procedures compared with MIGS.
This study included 2,625 providers from the CMS physician payment data who performed only traditional procedures (n=370), MIGS procedures (n=1727) or both procedure types (n=528) in 2019. The researchers used CPT codes to classify traditional and MIGS procedures. A multivariable linear regression model was created using certification year, rural-urban commuting area (RUCA) code—a metric of the Census Bureau that encapsulates the factors of population density, urbanization and daily commuting—and estimated income by practice zip code to predict the number and proportion of each type of glaucoma procedure.
The median number of MIGS procedures performed by each provider was greater in non-metropolitan areas (31 vs. 29), while the proportion of traditional procedures performed by each provider was greater in metropolitan areas (0.24 vs. 0.08). Regression analysis showed a positive relationship between certification year and the proportion of traditional procedures performed by each provider. Multivariate models found that certification year, RUCA code and estimated income of practice location were all significant predictors of the proportion of traditional procedures performed by each provider.
Physicians with a later certification year likely had more recent training, suggesting that there could be a connection between the timing of training and procedural preference.
“Since ophthalmologists who are not glaucoma subspecialists have a higher preference for MIGS, these findings suggest that glaucoma procedures performed in non-metropolitan areas are less likely to be done by glaucoma subspecialists,” the researchers wrote in their paper. “A possible explanation for this finding is that non-metropolitan areas have a lower number of subspecialists.”
The team did note that “the greater proportion of non-subspecialists among ophthalmologists with earlier training could explain the higher MIGS procedure preference among physicians with earlier certification years. However, the statistically significant relationship between certification year and the proportion of traditional vs. MIGS procedures may have limited value since the magnitude was small.”
The study concluded that more research is needed to better understand how this affects access and outcomes for different geographic regions and patient demographics.
| Click here for journal source. |
Xiao G, Boland MV. Comparing traditional and newer glaucoma procedures by physician experience and practice location in the United States. J Glaucoma. October 24, 2024. [Epub ahead of print]. |

