 |
|
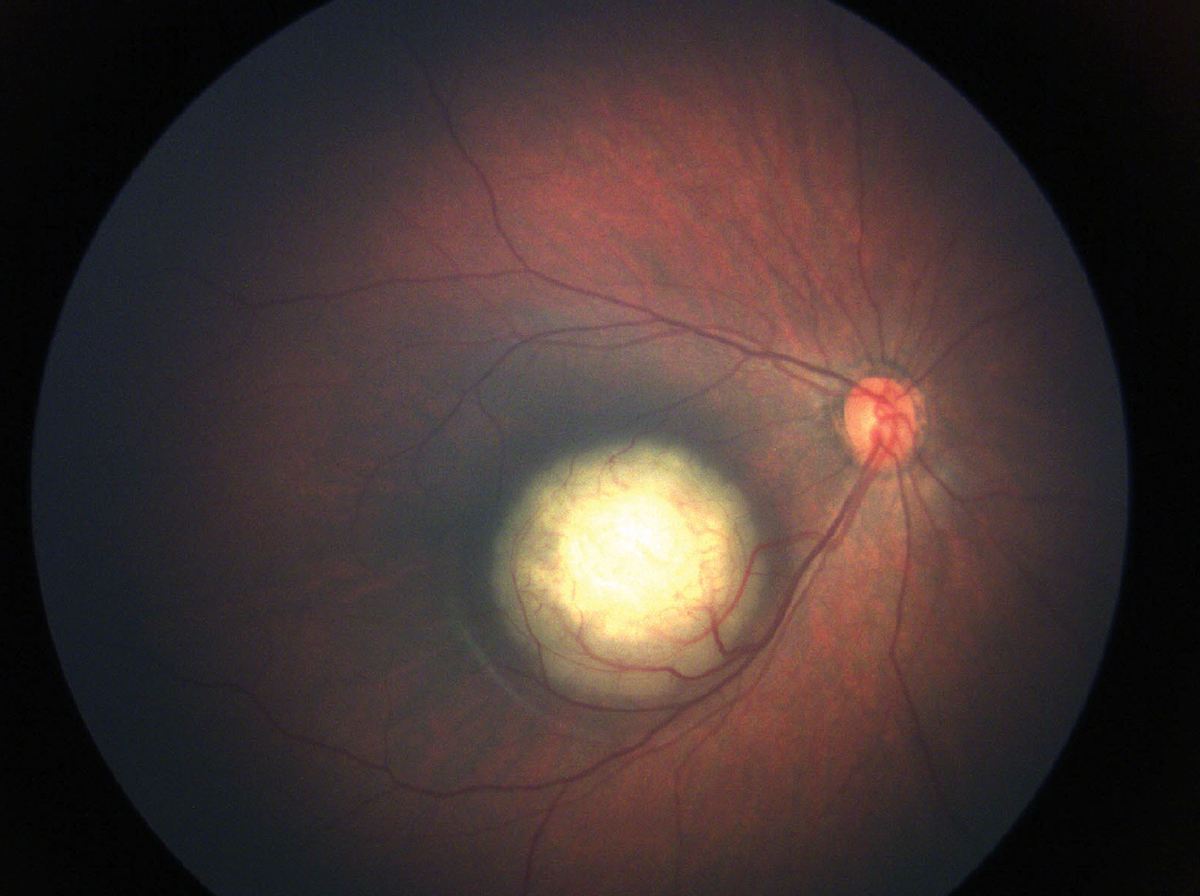
Children with retinoblastoma who received adjuvant chemotherapy after enucleation showed improved survival and reduced tumor recurrence, highlighting the importance of standardized treatment protocols. Photo: Julia Canestraro, OD. Click image to enlarge. |
Over the past 30 years, the prevalence of myopia in children and adolescents has increased from 24.3% to 35.8%. Recently published studies now include time periods encompassing the COVID-19
Findings from a multinational analysis of children with retinoblastoma supports the use of adjuvant chemotherapy after upfront enucleation and diagnosis of high-risk histopathology features (HRHF). The data, published in American Journal of Ophthalmology, also highlight the variations that exist across centers when defining HRHF and the need for a more standardized approach.
This retrospective clinical cohort study recruited children with retinoblastoma who underwent primary enucleation. “For analysis, only unilateral cases with standardized HRHF, defined as retrolaminar optic nerve invasion, massive choroidal invasion, scleral invasion, anterior-segment involvement and/or combined non-massive choroidal and prelaminar/laminar optic nerve invasion, were included,” according to the study authors.
The main outcome measures were orbital tumor recurrence, systemic metastasis and survival as well as number and outcome of cases converted to standardized HRHF. Six-hundred children who presented to 14 centers in nine countries were included in the study.
Of the total cohort, 505 children (84.2%) were classified locally as having HRHF and were treated with adjuvant chemotherapy. After a median follow-up period of 39.2 ±1.6 months, data showed that 6.0% had orbital tumor recurrence, 8.2% developed metastasis and 12.0% died. The researchers found that children who did not receive chemotherapy faced a significantly higher risk of orbital tumor recurrence, metastasis and death.
Additionally, 63 out of 600 children (10.5%) were initially deemed locally non-HRHF, but were converted to standardized high-risk histopathology features and included in the analysis. Among these, 9.5% had orbital tumor recurrence, 7.9% developed metastasis and 9.5% died.
The study authors reported isolated minor choroidal invasion with prelaminar/laminar optic nerve invasion in 114 children (19%); however, only 59.6% were locally considered HRHF. Six of these 68 children (5.3%) developed metastasis and subsequently died.
“In this multinational cohort of unilateral upfront enucleated retinoblastoma children demonstrating high-risk histopathology features, adjuvant systemic chemotherapy was beneficial, resulting in significantly reduced orbital tumor recurrence, metastatic spread, as well as improved survival rates,” the study authors wrote in AJO.
“Furthermore, the implications of not standardizing HRHF and defining protocols for adjuvant therapy result in adverse patient outcomes,” they concluded. “As efforts to address retinoblastoma on a global scale become evident, corresponding efforts to reduce disparities in retinoblastoma outcomes through defined management strategies are warranted, especially among lower income countries.”
| Click here for journal source. |
Arazi M, Baum A, Casavilca-Zambrano S, et al. Treatment Outcomes and Definition Inconsistencies in High-Risk Unilateral Retinoblastoma. Am J Ophthalmol. September 25, 2024 [Epub ahead of print]. |

