Many optometrists are active in the comanagement of cataract surgery. A multitude of surgical practices around the country involve the patients’ primary optometrists in the postoperative process. Receiving post-op care in a familiar setting by a doctor they know and trust allows the patient to feel comfortable during such a stressful event in their life. It also results in a smoother transition back to their routine eye care, where the management of patients’ other eye conditions can be continued without much interruption.
In order to maintain patients’ trust and confidence, optometrists must continue to be well-versed in the postoperative management of cataract surgery. Fortunately, many of the issues that arise during the postoperative process do not require surgical intervention and can be successfully addressed by optometrists. This article will act as a short step-by-step guide to help you stay up-to-date and be able to anticipate postoperative issues in the order they generally arise.
Early Post-op Period (One to Four Days)
 |
| ODs can contribute to post-op cataract care by adopting a few simple procedures to allow for appropriate observation. Click image to enlarge. |
Some studies have questioned the need for a one-day post-op visit after uncomplicated cataract surgery, given the expected low risk of complications.1 However, it is still part of many surgeons’ postoperative protocols. There are several important things that need to be assessed at this early visit.
First, evaluate the eye for a wound leak. Cataract surgery may be performed through either a corneal, limbal or scleral incision. Clear corneal incisions (CCIs) have become a lot more common than scleral tunnel incisions over the last two decades.2 While CCIs have their advantages, they are inherently weaker and are more likely to be leaky.3 “Painting” the incision site with a fluorescein strip to check for a Seidel sign would help identify a leaky wound. Mild leaks that are present a day after surgery often seal themselves.
Temporarily stopping steroid drops, adding an aqueous suppressant and placing a bandage contact lens over the eye may help the incision seal quicker. In more severe cases, such as when intraocular pressure (IOP) is in the low single digits or the anterior chamber is flat or shallow, sending the patient back to the surgeon for wound resuturing is indicated.
Corneal edema may occasionally be present early on after cataract surgery. While it resolves on its own in the majority of cases, it can be a cause for concern for patients, many of whom expect better vision immediately post-op. Complicated surgery, advanced cataracts, underlying endothelial dystrophy, uveitis and endothelial trauma all can increase the risk of post-surgical corneal edema.4 Reassure patients regarding the temporary nature of this issue. It is safe and effective to use 5% sodium chloride as an adjunct for faster corneal recovery.5
A common early complication of cataract surgery is IOP spike. This is generally a self-limiting phenomenon and often resolves within 24 to 48 hours after surgery. Patients with healthy optic nerves tolerate these IOP spikes well without any noticeable optic nerve damage. Patients who have glaucoma tend to experience postoperative IOP spikes more frequently and are very susceptible to additional nerve damage.6 Generally, if IOP is 30mm Hg or above, initiate ocular anti-hypertensive medications (such as brimonidine, timolol and/or dorzolamide). Use oral acetazolamide in cases of extremely high IOP. Monitor the patient in the clinic to make sure the IOP is decreasing and then give them IOP-lowering drops to use at home. In most cases, IOP-lowering medication is not needed past a week and is discontinued at the next follow-up after control over IOP is achieved.
A day-one post-op visit is also useful because it offers another opportunity to go over postoperative precautions, medication regimen and allows the patient to ask questions while being in the thick of it. Patients may report some discomfort in the first few days after the surgery. Some soreness and tenderness might be present for a day or two, usually improving noticeably with every sleep. If discomfort is significant, a short course of oral acetaminophen or ibuprofen may be helpful. Inflammation can cause light sensitivity, so recommend sunglasses for when outside. Strenuous physical activity, makeup use and exposure to sitting water and other unclean environments should be avoided.
A typical postoperative medication regimen varies somewhat clinic to clinic but generally includes an antibiotic, a steroid and a non-steroidal anti-inflammatory (NSAID). These medications are commonly prescribed to patients in the form of eye drops, though they can also be administered via injection into the eye during the surgery. Referring optometrists should familiarize themselves with the medication regimen preferred by the surgical center that they work with in order to maintain good continuity of care.
In uncomplicated cases, the additional use of an NSAID drop may not bring about much benefit over using steroids alone, but in more complex cases, such as in patients with diabetes, uveitis and retinal and epiretinal issues, an NSAID may lower risk of cystoid macular edema (CME).7 Antibiotic drops are usually used for one week, while anti-inflammatory drops are usually continued for three to four weeks. Some practices initiate a steroid taper a couple of weeks after the surgery, while others recommend that the patient maintain initial frequency until the end.
Ocular surface discomfort, ranging from foreign body sensation to stinging, may last for two to four weeks, gradually improving. This generally results from the surgical stress to the eye and is more pronounced in patients with pre-existing dry eye issues. Copious artificial tears will help mediate such symptoms. Educate patients that cataract surgery may cause a temporary worsening of their dry eye. A course of cyclosporine or lifitegrast may be helpful to get symptoms under control.
Subconjunctival hemorrhages are also common, especially with scleral tunnel incisions, where conjunctival tissue is altered. In patients who take blood thinners or have a clotting disorder, the hemorrhages may be more pronounced. These do not require treatment apart from reassurance and education, and are usually fully resolved after two weeks.
Intermediate Post-op Period (Five to 14 Days)
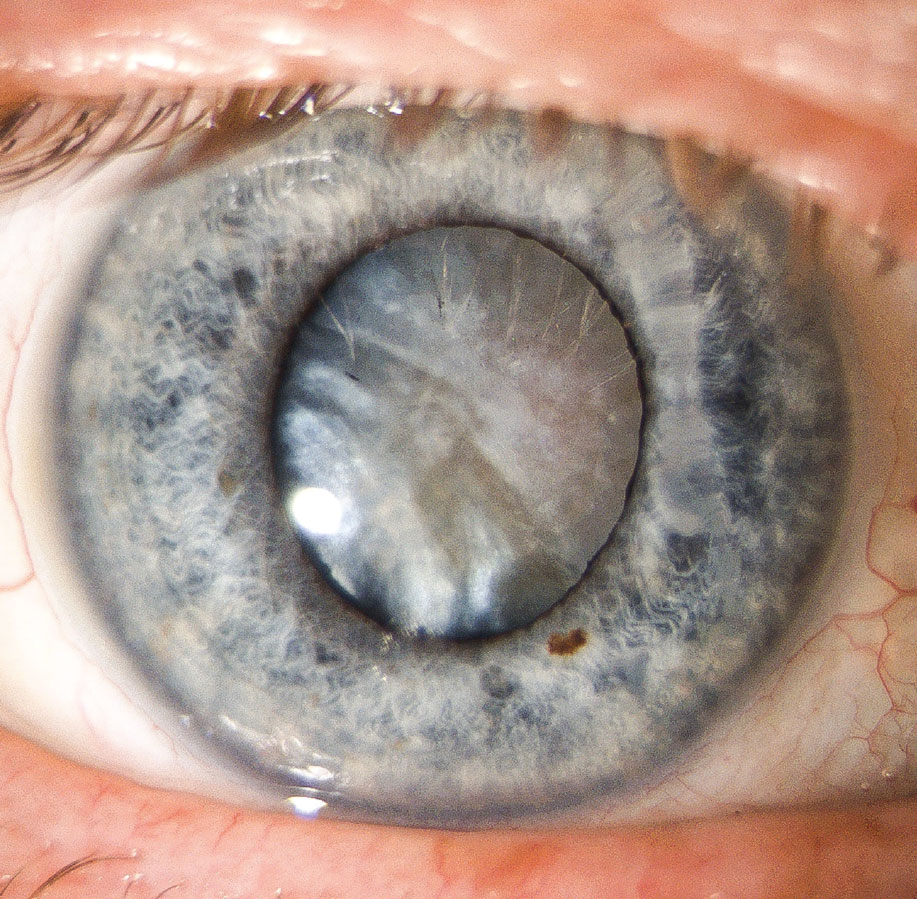
 |
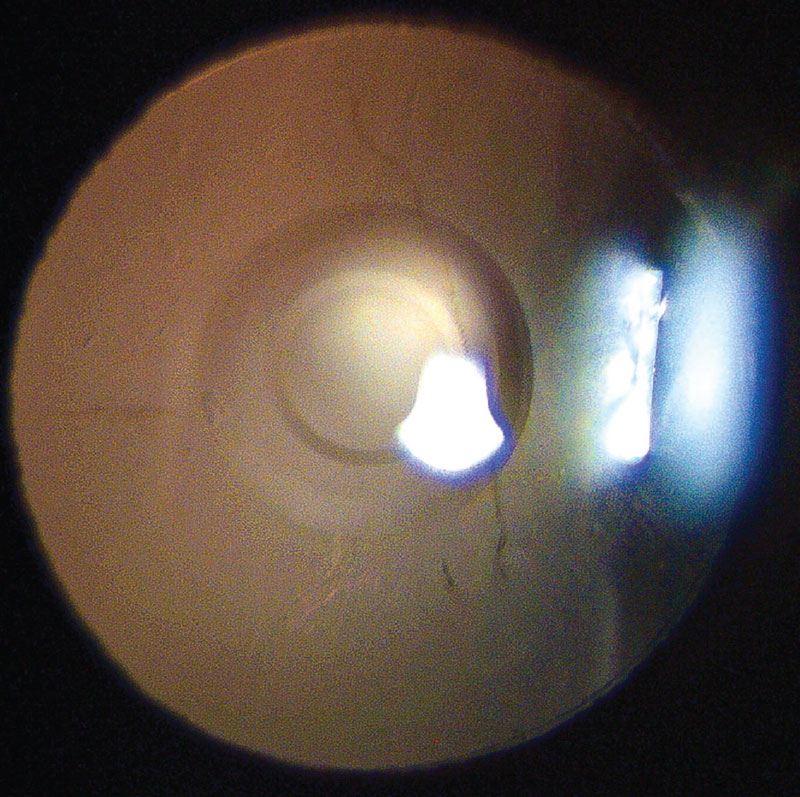
| Nuclear fragments post-op require surgical removal. Click image to enlarge. |
One of the most serious complications of cataract surgery, endophthalmitis, usually presents seven to eight days postoperatively.8 The incidence of acute endophthalmitis after cataract surgery has been steadily decreasing over the last few decades, and though it is incredibly rare, there has been an uptick with transition from scleral tunnel to clear corneal incisions.9
Patients who have acute postoperative endophthalmitis typically present with symptoms of blurry vision, red eye and severe pain. Dilated examination is important when such symptoms are reported. Vitreous inflammation will be obvious upon examination. A hypopyon is also present in many cases.10 If endophthalmitis is suspected, notify the cataract surgeon immediately and refer to a retinal specialist for urgent treatment.
Occasionally, a small bit of lens may be left in the eye after the surgery. It may not be apparent at first, hiding behind the iris, but later may make its way into the anterior chamber. If the fragment is white and very fluffy, it is likely cortical. Small cortical fragments may resolve on their own with increased anti-inflammatory regimen. Increasing the steroid drop to every two hours schedule for a week or two may help resolve this issue. If the fragment larger or made of nuclear material (more yellow/brown and smooth), surgical removal is necessary. Whenever lens fragments are found, it is best to check with the surgeon regarding further management.
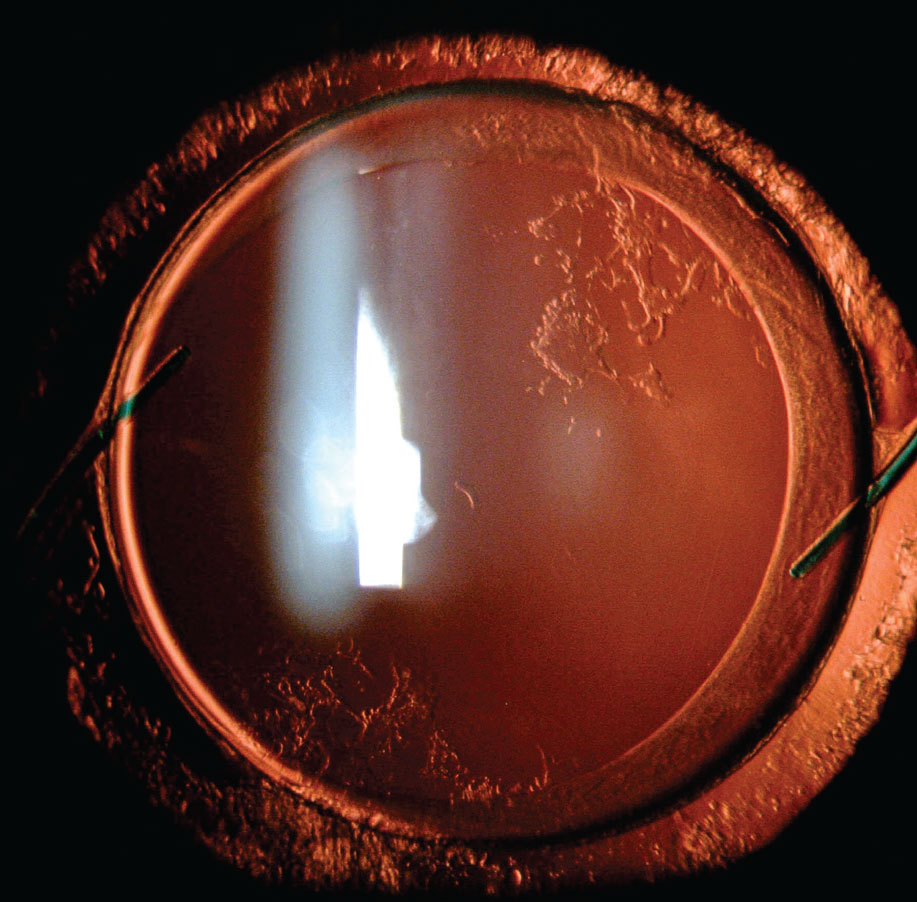 |
| Posterior capsular opacification may present months or years after cataract surgery and require YAG laser capsulotomy. Click image to enlarge. |
If a patient had significant corneal astigmatism, they may have received a toric intraocular lens (IOL). Toric IOLs have a small risk of rotation after the surgery, potentially resulting in subpar vision. The rotation is most likely to occur in the first week after the surgery.11 It is best to verify toric IOL positioning one to two weeks postoperatively with a dilated exam. If the lens is in the right position, it is unlikely to rotate in the future. If the patient’s uncorrected vision is blurry and significant residual astigmatism is present, the patient should be sent back to the surgeon for an IOL rotation. IOL rotations are best performed within the first few weeks after the initial cataract surgery.
Late Post-op Period (Two Weeks or More)
A complication with a more delayed onset is postoperative CME (also known as Irvine-Gass syndrome). It occurs about 1% to 2% of the time and usually takes several weeks after the surgery to develop.12
The risk of CME is higher in eyes with history of epiretinal membrane, retinal surgery, uveitis and in eyes that undergo a more complicated cataract surgery. It is best detected with a macular OCT and is usually identified when patient’s vision does not seem to match pre-surgery potential acuity. In the majority of cases, a combination of topical steroid and topical NSAID will result in complete resolution within a few weeks. Dilate all patients at the monthly follow-up to rule out CME, as well as any retinal tears or detachments.
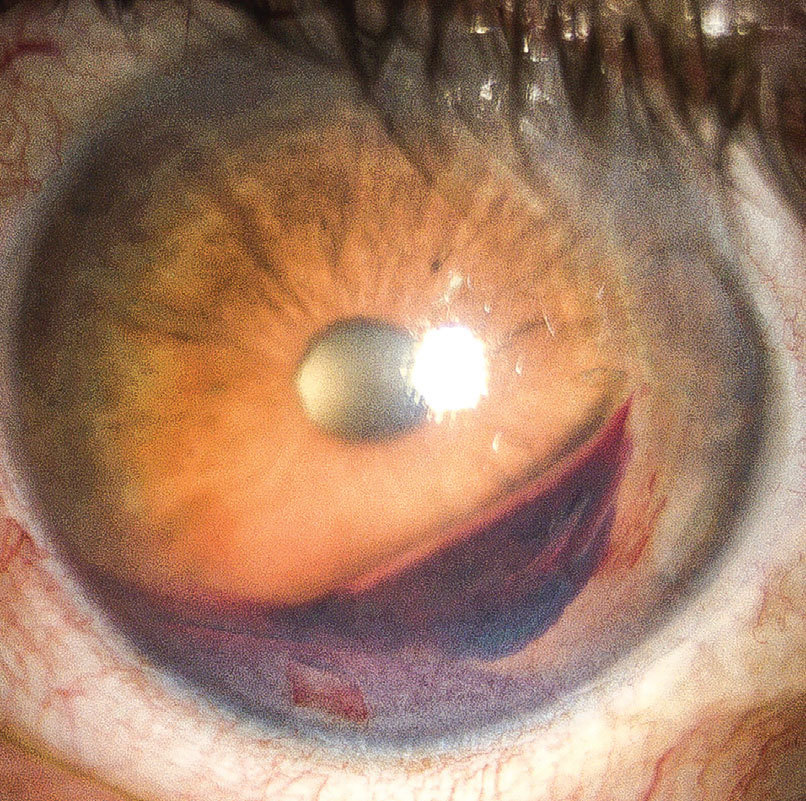 |
| If hyphema is mild, increasing the steroid dosage may help it clear faster. Click image to enlarge. |
Dysphotopsia is a term to describe a range of unwanted visual phenomena that result from light reflecting off the IOL onto the retina.13 Dysphotopsias can be positive, such as bright artifacts, flickering lights or halos, or negative, such as shadows or dark areas of visual field. Dysphotopsias are most noticeable in the temporal field of vision and are often described by patients as a crescent, line or hair.
While dysphotopsias are commonly noted in the first few weeks after cataract surgery, they rarely persist long-term.14 This is largely due to neuroadaptation, when neural plasticity of the visual cortex allows it to ignore unwanted visual phenomena.15 The management of such symptoms mostly consists of education and reassurance that the visual disturbances will disappear on their own; however, the process of neuroadaptation may take up to six months.
In a small number of people, dysphotopsia may remain bothersome months after cataract surgery. In those cases, send the patient back to the surgeon for consultation and discussion of options, which may include additional surgical treatment.
Minimally Invasive Glaucoma Surgeries (MIGS)
Cataract surgery is becoming increasingly intertwined with glaucoma procedures. Given that a large number of cataract patients also have glaucoma, these conditions are tightly aligned. Multiple MIGS procedures that are performed at the time of cataract surgery range from device implantation, such as the iStent Inject (Glaukos) or the Hydrus (Ivantis), to canaloplasties, such as the Omni surgical system (Sight Sciences) and iTrack (Ellex).
Evaluate physically implanted devices with gonioscopy one to two weeks postoperatively, to make sure appropriate stent positioning. Trabecular meshwork-bypass stents are most commonly placed in the nasal quadrant, due to a higher concentration of collector channel entrances in that area.16 It is best to avoid gonioscopy in the first week post-op to avoid applying pressure on the eye.
Causes of stent occlusion may include blood clots early after surgery or peripheral anterior synechiae in the months after the procedure. After surgery, it is recommended to remove glaucoma medications one by one in order to arrive at the minimum amount of drops necessary to maintain IOP at target.
Hyphema is not uncommon in the first week after the procedure.17 If hyphema is mild, no additional treatment is necessary. If hyphema is severe, a washout of anterior chamber may be needed, so further management of these patients should be discussed with the surgeon.
Presbyopia-correcting IOLs
 |
| The Vivity IOL is one newer option for patients who want to limit their dependence on spectacles. Click image to enlarge. |
An increasing number of patients opt for presbyopia-correcting IOLs in order to have greater spectacle independence after cataract surgery. The last few years have witnessed a wave of new IOL designs becoming available in the United States: the Symfony and Synergy IOLs by Johnson & Johnson Vision and the PanOptix IOL and Vivity IOL by Alcon. Performance of presbyopia-correcting IOLs has improved drastically and more patients are candidates for such lenses, but there are still a few things to watch for.
The success of premium IOLs depends more on education and counseling prior to surgery than on postoperative measures. Postoperatively, these patients may have higher expectations. It can take between one and four weeks for the visual acuity to reach optimal levels.
Each IOL has unique characteristics and differentiating between them is a topic for another article. To sum it up, most multifocal or extended depth-of-focus (EDOF) IOLs have diffractive rings designs, which may cause patients to see halos around lights in the dark. These are much less bothersome than those experienced with older generation lenses but can still cause issues for a small percentage of patients. Reassure patients that halos improve with neuroadaptation and encourage them to give it some time. Such symptoms greatly diminish over four to six months after the surgery.
The most common causes of dissatisfaction in patients with presbyopia-correcting IOLs are residual refractive error, dry eyes and halos, in that order.18 Refractive outcome is usually determined a month after the surgery. Manifest refraction should be done if the visual outcome is unsatisfactory. If significant residual refractive error is detected, send the patient back to be evaluated for surgical options—either a refractive procedure or an IOL exchange.
Takeaways
Optometrists are increasingly involved in the postoperative management of cataract surgery. Due to the continually evolving nature of this field, the onus is on us to keep up with best practices, technological advancements in order to serve our patients better.
Dr. Sukhovolskiy is a staff optometrist at Pacific Cataract and Laser Institute, practicing in Tacoma, WA. He has no financial disclosures.
1. Kessel L, Andresen J, Erngaard D, et al. Safety of deferring review after uneventful cataract surgery until two weeks postoperatively. J Cataract Refract Surg. 2015;41(12):2755-64. |