The Do’s & Don’ts of Oral Medication
Understanding when and how to prescribe oral medications will help optometrists provide optimal patient care.
By Jane Ann Grogg, OD
 |
Release Date: March 15, 2020
Expiration Date: March 15, 2023
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
- Describe indications of common oral medications in eye care.
- Prepare for precautions and drug interactions.
- Recognize the importance of taking a good medical history.
- Monitor patients on oral therapy for adverse events.
- Discuss proper prescribing practices.
- Identify when to refer and how to consult with other specialties.
Target Audience: This activity is intended for optometrists engaged in the care of patients requiring oral medications.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by the Postgraduate Institute for Medicine and Review Education Group. Postgraduate Institute for Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education, and the American Nurses Credentialing Center, to provide continuing education for the healthcare team. Postgraduate Institute for Medicine is accredited by COPE to provide continuing education to optometrists.
Faculty/Editorial Board: Jane Ann Grogg, OD.
Credit Statement: This course is COPE approved for 2 hours of CE credit. Course ID is 67116-PH. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Dr. Grogg has nothing to disclose.
Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
13th Annual Pharmaceuticals ReportCheck out the other feature articles in this month's issue: |
The use of oral medications in optometry broadens our scope of practice and provides more comprehensive care. While topical medications treat a wide variety of ophthalmic disorders, we need to recognize when oral medications are a better option. Knowing when an oral medication is indicated and the proper dosing schedule are crucial.
Choosing effective medication is important to ensure prompt and adequate resolution of a patient’s problem. You can select medications with fewer side effects and familiarize yourself with common adverse events to help with compliance. Patients who know what to expect will be less likely to call the office with concerns or stop taking the medication because they were surprised by a side effect.
Cost is always a potential issue for patients. While this cannot be a deterring factor in providing the best care for patients, less expensive generic equivalents, when available, should be considered.
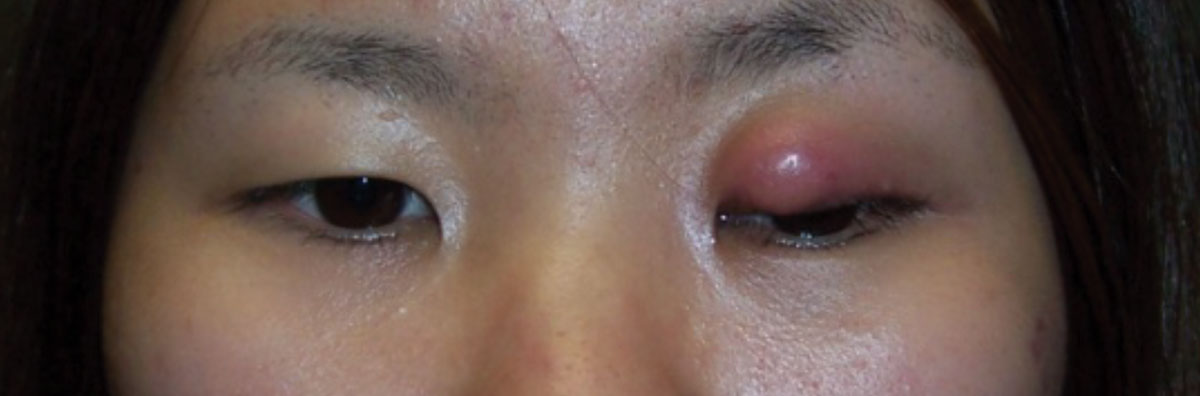 |
| Fig. 1. This patient with preseptal cellulitis required oral antibiotics. Click image to enlarge. |
Patient assessment begins with history, which is critical in shaping our differential diagnosis and management. In addition, a good medical history is critical to confirm the necessity of oral medications as well as to determine the risk of allergic reaction and cross-sensitivities to other medications.
From the moment you begin taking the patient’s history, your wheels should be turning. A good medical history will inquire about current systemic medical conditions that could affect liver and kidney function. Oral medications usually metabolize through the liver or kidney, and you may have to adjust the dosing depending on the patient’s creatinine clearance level or liver disease. Patients must be monitored for the potential for adverse events.
Antibiotic Therapy
When deciding on oral antibiotics, you must know how to choose between the various classes, including penicillinase-resistant penicillin, broad-spectrum beta lactamase inhibitor, macrolide, cephalosporin, quinolone and tetracycline. You should be comfortable and experienced with at least one option in each class of antibiotics.
A common indication for oral antibiotics is for the treatment of preseptal cellulitis (Figure 1). This is often the result of infected soft tissue originating from an infected meibomian gland. Warm compresses are always an important adjunctive therapy, but oral antibiotics may be necessary to clear the infection and prevent further complications.
When treating eyelid infections, choosing a penicillinase-resistant penicillin for effective treatment is critical since bacteria produce an enzyme called penicillinase, which renders penicillin ineffective.
 |
| Fig. 2. In this case of an orbital blowout fracture, oral antibiotic therapy was used to prevent the possibility of orbital cellulitis. Click image to enlarge. |
Dicloxacillin belongs to the class of penicillinase-resistant penicillins and is listed as a first-line therapy in the Sanford Guide to Antimicrobial Therapy.1 The recommended dosage is 250mg four times a day for severe infection or 125mg four times a day for mild to moderate cases. In general, it is a well-tolerated antibiotic; however, the frequent dosing schedule may make compliance difficult.
Many clinicians prefer antibiotics that can be dosed once or twice a day to improve compliance. Gastrointestinal (GI) upset and the risk of C. difficile is listed as an adverse reaction and is a ubiquitous side effect with many oral antibiotics.
Another common antibiotic used in the treatment of soft tissue infection is a broad-spectrum penicillin and beta lactamase inhibitor known as Augmentin (amoxicillin and clavulanic acid, GlaxoSmithKline). The beta lactamase inhibitor renders this antibiotic penicillinase-resistant, thus it can be used in eyelid infections. The dose is based on the amoxicillin component, with a typical dose being 500mg every 12 hours. For more severe infection, the dosing is every eight hours. Using amoxicillin without the clavulanic acid component may result in treatment failure due to the lack of the beta lactamase inhibitor.
Of the cephalosporins, first-generation Keflex (cephalexin, Hikma) is a potential choice for the treatment of preseptal cellulitis as well. A typical dose for a mild case would be 500mg every 12 hours. For more severe infections, this could be dosed up to three times a day.
Allergic cross-sensitivity to cephalosporin products is a listed risk in patients who are allergic to penicillin. This risk is likely overestimated and, for the most part, largely ignored unless the patient has had an anaphylactic reaction.
A true IgE-mediated anaphylactic reaction includes hypotension, laryngeal edema, wheezing, angioedema or urticaria. Sorting out the type of reaction the patient is reporting as an allergic reaction is critical. Too often patients confuse other side effects of the drug (such as stomach upset) with an allergic response. The potential for this cross-sensitivity may be related to the chemical side chain of certain cephalosporin drugs being similar to that of penicillin agents.2
Usually, second- or third-generation cephalosporin agents with dissimilar side chains from penicillin have a low chance of cross-reactivity in IgE-mediated reactions. Commonly used cephalosporin agents with dissimilar side chains include: Ceftin (cefuroxime, GlaxoSmithKline), Vantin (cefpodoxime, Pfizer), Cefzil (cefprozil, Bristol-Myers Squibb) and Omnicef (cefdinir, AbbVie).
The recommendation is to avoid cephalosporins with similar side chains (first generation such as cephalexin, cefadroxil) if the patient has experienced an anaphylactic reaction to the penicillin class. If a patient experiences a non-anaphylactic reaction, the risk of cross-sensitivity and subsequent allergic response may be quite low. However, all cephalosporin drugs will have this risk listed as a contraindication.
 |
| Fig. 3. This patient with culture-positive HSV keratoconjunctivitis of the left eye (note herpetic lesions on temple) was treated with oral antiviral therapy and received a narcotic for pain. Click image to enlarge. |
If a patient is allergic to a penicillin and you wish to avoid the cephalosporin class, a macrolide is a good alternative. A commonly prescribed macrolide is azithromycin. This antibiotic is well tolerated and generically available. It has a long half-life, which makes the dosing schedule easy. This, in turn, helps with compliance. It can be prescribed as two 250mg tablets on day one followed by 250mg daily for an additional four days, originally known as a “Z-pak.” This long-acting antibiotic continues to provide coverage for several days despite its short five-day course. There is also a three-day azithromycin package which consists of three 500mg tablets.
Azithromycin is also the treatment of choice for chlamydia infections. The recommended dosage is a 1g dose given as two 500mg tablets.
For patients who have a difficult time swallowing pills, a good option is a 1g powder that can be dissolved in water or juice. A positive chlamydia culture will trigger the Health Department to follow through to ensure proper treatment of the patient as well as sexual partners. You should also consider referring the patient for other sexually transmitted disease testing as well as safe-sex counseling.
Bactrim (trimethoprim/sulfamethoxazole, Roche) is listed as an alternative for patients with penicillin allergy and is of the sulfonamide class. It is also considered a first-line therapy for methicillin-resistant Staphylococcus aureus (MRSA) infections. This antibiotic interacts with oral anticoagulants, hypoglycemics, diuretics and tricyclic antidepressants, to name a few.
Additional adverse reactions include blood dyscrasias, pancreatitis and rash, and you should consider any interactions and avoid prolonged administration. The double-strength version contains 800mg of sulfamethoxazole and 160mg of trimethoprim. It is dosed as one tablet every 12 hours for a week, depending on the type of infection.
| Prescribing Best Practices Proper prescribing practices include specifying the milligram dose of the medication, the number of tablets or capsules (should be equal to the number of days and frequency the patient is taking the medication) and prescription instructions for both the pharmacist and the patient. While Latin abbreviations are still acceptable, the more common practice is to simply write (or e-prescribe) the prescription longhand to avoid medical mistakes. For instance, QD is often disallowed in the hospital setting because of the common confusion with QID. You should consider the possibility of pregnancy and lactation in all women of childbearing age. As of 2015, the FDA replaced the assigned risk letter system (categories A, B, C, D and X) with the Pregnancy and Lactation Labeling Final Rule (PLLR) for all prescriptions. This narrative is meant to be more informative and meaningful to both the provider and individual patient. In turn, it allows for better individualized patient-directed counseling. The rule also includes a subsection called Females and Males of Reproductive Potential, which provides information about pregnancy testing, birth control and effect on fertility. Medications submitted to the FDA as of 2015 must use this format. Drugs approved on or after June 30, 2001 will be phased in gradually. Those approved prior to that are not subject to the PLLR rule but will have the letter category removed. |
The quinolone class, such as Levaquin (levofloxacin, Janssen), offers an easy dosing schedule of 500mg once daily for seven to 10 days for uncomplicated skin and skin structure infection. However, this class of antibiotics carries a black label warning for tendinitis and tendon rupture as reported in the literature.3 This risk is in all ages, though patients older than 60 have an increased risk as do those taking corticosteroid and patients with kidney, heart or lung transplants. This class should also be avoided in patients with myasthenia gravis. Given the gravity of these complications, the quinolone class should really be limited to those patients who have no alternative treatment options.
The last class of antibiotics, for the purposes of this article, is tetracyclines. Within this class, doxycycline is commonly prescribed because of the ease of dosing compared with tetracycline. Doxycycline has fewer reported adverse effects than minocycline, but prescribing may come down to doctor preference.4 Keep in mind the extended release versions of these drugs, while having less GI side effects, can be more expensive.
Tetracycline is often the treatment option for chronic meibomian gland dysfunction (MGD). The available treatment options for patients suffering from chronic MGD have greatly expanded, but sometimes an oral medication for adjunctive treatment is beneficial. Generally speaking, we use doxycycline for its anti-inflammatory properties at lower doses. It may be necessary to use doxycycline for several weeks or months to treat the chronic condition of meibomianitis. Often starting with a dose of 50mg once or twice daily for a couple of weeks can then be maintained at 50mg daily for several weeks. This is typically done with adjunctive therapy such as warm compresses and lid scrubs, at a minimum.
Recommending the patient take this medication with food will help ease the GI side effects. In addition, doxycycline can cause a patient to sunburn more easily and can cause esophagus reflux. Advising the patient not to lay down after taking doxycycline may help minimize this side effect.
Doxycycline, in combination with a topical corticosteroid, is also known to aid in the prevention of recurrent corneal erosions. Research suggests this works by inhibiting the extracellular matrix metalloproteinases which are responsible for non-adhesion of the epithelium once traumatized.5,6
Current clinical practice guidelines for patients with MRSA recommend increasingly aggressive treatment with increased infection severity.7 The list of antibiotics known to be effective in MRSA infection includes trimethoprim-sulfamethoxazole, tetracyclines and clindamycin. Other possible oral agents include oxazolidinones, delafloxacin and the tetracycline omadacycline, but cost can be substancial for these agents.
 |
| Fig. 4. This patient with herpes zoster ophthalmicus was successfully managed with an antiviral therapy. Click image to enlarge. |
Other indications for oral antibiotics in optometric practice include dacryocystitis and prophylactic coverage in orbital blowout fractures, although the latter tends to be controversial (Figure 2). When considering the use of an oral antibiotic prophylactically in orbital blowout fractures, consider consulting with an oculoplastic surgeon.
These are just some of the recommended antibiotics and scenarios to consider when the need for oral antibiotics arises in the optometric setting. You can identify other antibiotic options through resources such as the Monthly Prescribing Reference or by consulting infectious causes in the Sanford Guide to Antimicrobial Therapy.1 The Sanford Guide is updated yearly and is beneficial in guiding the standard of care in the medical community.
Antiviral Therapy
This plays a significant role in preventing or minimizing complications related to herpes simplex virus (HSV) and herpes zoster virus. Oral antivirals work to hasten the resolution of these conditions, reduce viral shedding and help prevent the formation of new skin lesions. They can help decrease both the incidence and severity of ocular complications.
When treating herpes zoster, recommend treatment within 72 hours of vesicles erupting. Instituting treatment within this timeframe not only reduces the duration and severity of the acute pain but may also lessen the risk of progression to post-herpetic neuralgia and other long-term complications and subsequent vision loss.8-10 Post-herpetic neuralgia occurs as frequently as 50% of the time in patients with herpes zoster opthalmicus.11
Herpes simplex lesions may present on the eyelid or at the mucocutaneous border (Figure 3). These typically present with localized vesicular lesions that ulcerate and are painful. When the vesicles rupture, you can see a shallow ragged ulcer.
Three commonly used antiviral medications are acyclovir, valacyclovir (the prodrug of acyclovir) and famciclovir. All of these are generically available and reasonably priced. The latter two offer less frequent dosing schedules and may help to improve compliance.
For herpes zoster ophthalmicus, the recommended dosing is as follows: acyclovir 800mg five times a day, valacyclovir 1g three times a day and famciclovir 500mg three times a day. An easy way to remember the dosage for herpes simplex virus is simply to divide the zoster dose in half (Figure 4).
Oral antiviral therapy is also an effective approach for herpetic keratitis. Practitioners may choose this avenue of treatment if topical antiviral medication is not readily available or not affordable. In fact, oral antiviral therapy is the treatment of choice for children.12
Oral antiviral therapy can suppress recurrence of herpetic disease, according to the Herpetic Eye Disease study. The recurrence rate of any form of ocular HSV infection was reduced by 41%, and a 50% reduction in the rate of recurrence of stromal keratitis was observed.13 The study used acyclovir 400mg twice a day. Valacyclovir is equally as effective at immune suppression with a dose of 500mg twice a day.14
HSV has been implicated in, among others, cranial nerve VII paresis with studies indicating a likely association (Figure 5).15-17 The Sanford Guide suggests treating Bell’s palsy with oral prednisone and oral antiviral therapy if no other causative condition is suspected.1 The addition of 60mg to 80mg of prednisone with a 20mg taper over several days is recommended if diagnosed within 72 hours of onset.
Overall, oral antiviral therapy is generally well tolerated by patients, as the drug is site specific. Some side effects may include GI disturbance, headache, vertigo, malaise and central nervous system (CNS) disturbances (especially in the elderly).
Steroids
These play a role in the management of many ocular diseases, including contact dermatitis, eczema, temporal arteritis, orbital inflammatory pseudotumor, Bell’s palsy, Graves’ disease, orbital floor fractures, optic neuritis and chronic uveitis (Figure 6). The only true contraindications for oral steroid use are systemic fungal infection, live vaccinations and drug hypersensitivity.
However, you should be cautious when prescribing them in the presence of peptic ulcer disease, diabetes, tuberculosis, active infection, psychosis and pregnancy. Know what you are treating without disseminating infection or masking pain.
Side effects of oral steroids include hyperglycemia, hypokalemia, hypertension, peptic ulcer, increased intraocular pressure, cataract, benign increased intracranial hypertension, mental status changes, osteoporosis, decreased wound healing and fluid retention, to name a few. You can add a proton pump inhibitor with oral prednisone to minimize the GI side effects.
 |
| Fig. 5. This patient’s cranial nerve VII palsy, presumed to be caused by herpes simplex, was managed with prednisone and antiviral therapy. Click image to enlarge. |
 |
| Fig. 6. Oral prednisone was used to manage this patient with contact dermatitis. Click image to enlarge. |
Pain Medications
Occasionally, acute care management requires oral pain medications when topical therapy is not adequate. The scope of our management runs the gamut from palliative agents such as artificial tears and cold compresses to prescription opioids, depending on the individual state laws. You must document the quality and extent of the patient’s pain and pair that with the clinical picture to make judgement calls on their medical need. It is essential to identify the source of the pain, manage the patient effectively and treat the causative problem to avoid masking pain.
Corneal problems are the most common source of ocular pain and often the most intense because of the cornea’s high density of nerves. When the eye is traumatized, the patient often experiences eyelid edema, tearing and photophobia. Secondary anterior uveitis may develop as an additional source of discomfort and inflammation.
Oral pain medication options can be divided into non-narcotic and narcotic medications. Non-narcotic options include analgesics, non-steroidal anti-inflammatory drugs (NSAIDs) and cox-2 inhibitors. A common over-the-counter analgesic is acetaminophen. It is available in multiple dosages, starting at 325mg with an extra-strength version of 500mg. This medication can be dosed every four to six hours for a maximum of 3g daily. In 2011, the FDA asked drug manufacturers to limit the strength to 325mg tablets and to reduced the maximum recommended amount to 3g per day from the previous 4g per day.
Acetaminophen is contraindicated in liver disease, alcoholism and acetaminophen hypersensitivity. It is commonly paired with opioids to potentiate their effect, improve efficacy of the opioid and allow less narcotic to be prescribed.
Oral NSAIDs are contraindicated in aspirin allergies and should be used with precaution in active peptic ulcer or GI disease, renal or liver impairment, heart failure, edema and hypertension. Adverse reactions include gastrointestinal ulcer/bleeding/upset, headache, dizziness, fluid retention, rash, pruritus and tinnitus. Asthma patients have an increased risk of allergy to NSAIDs.
When used at lower doses, NSAIDs have pain management benefits; at higher doses they have anti-inflammatory benefits. Oral NSAIDs may help with ocular surface injuries, moderate to severe episcleritis, mild scleritis and uveitis. Ibuprofen is dosed 200mg to 800mg every four hours for a maximum dose of 3,200mg daily; however, the side effect profile is better with a maximum dose of 1,600mg daily.
Naproxen, available over the counter, is given in 220mg tablets. The initial dose is two tablets, followed by one tablet every eight to 12 hours for a maximum of three tablets in 24 hours. Prescription-strength dosage is available in 250mg, 375mg and 500mg, though the lowest effective dose for the shortest duration is advisable.
 |
| Fig. 7. This patient who had blunt trauma with hyphema, corneal and conjunctival abrasions, anterior uveitis and iris sphincter tears received an adjunctive oral narcotic for three days. Click image to enlarge. |
NSAIDs carry a black box warning of increased risk of serious and potentially fatal cardiovascular thrombotic events, including myocardial infarction and stroke, which may occur early in treatment and may increase with duration of use. There is also a black box warning of serious and potentially fatal GI adverse events including bleeding, ulcer and stomach or intestinal perforation.
Alternating acetaminophen with ibuprofen every two hours is often an effective means of managing mild to moderate pain. These medications, which employ two different pathways for pain management, are typically readily available and most patients already have these medications in their homes.
Narcotics in acute pain management are reserved for when topical management is not adequate or contraindicated (Figure 7). Narcotics range from schedule I to V (more to less addictive). Most are prescribed as a ratio of the narcotic and the acetaminophen in each tablet. For example, hydrocodone/acetaminophen 5/500 contains 5mg of hydrocodone bitartrate and 500mg of acetaminophen with a recommended dose of one or two tablets every four to six hours as needed for pain.
Ultram (tramadol, Johnson & Johnson) is a schedule IV narcotic with an adult dose of 50mg to 100mg every four to six hours as needed for moderate and moderate-severe pain.
Alternatively, Ultracet (acetaminophen/tramadol, Janssen Pharmaceuticals) contains 325mg of acetaminophen with a slightly lower dose of tramadol (37.5mg). It is dosed two tablets every four to six hours with a maximum of eight tablets per day for up to five days.
With all centrally acting agents, precaution should be used in patients with a history of seizure disorders, head injury or respiratory depression. Adverse reactions may include dizziness, nausea, constipation, headache, somnolence, GI upset, dry mouth, itching and CNS stimulation.
Remember to warn patients of alcohol use or other CNS depressants, as the CNS depression is addictive. An example is the combination of benzodiazepines and narcotics, which carry the risk of opioid-related death.
Given the current opioid epidemic and widespread opioid abuse, you should prescribe the least amount of narcotic possible to achieve the desired pain relief. Do not prescribe beyond the number of days the pain is severe enough to warrant opioids. Always reevaluate and adjust based on clinical findings. Be vigilant of drug-seeking behavior in patients who claim to have eye pain inconsistent with the clinical examination. The use of state-based prescription drug monitory programs helps to identify patients at risk of addiction or overdose.
With a good medical history and a careful understanding of each medication’s indications, contraindications and potential side effects, you can safely treat patients using any number of oral medications. If the patient does not respond or worsens on treatment, don’t be afraid to refer.
Ultimately, optometrists must embrace this therapeutic privilege. By doing so, we will be using the privilege that we fought to obtain, which is important in the continued growth of our profession.
Dr. Grogg is the director of the Indiana University Health Center Eye Clinic and a clinical professor of Optometry at Indiana University School of Optometry in Bloomington, Indiana.
1. The Sanford Guide to Antimicrobial Therapy 2019. Sperryville, VA: Antimicrobial Therapy, Inc. 2. Pichichero ME. Cephalosporins can be prescribed safely for penicillin-allergic patients. J Fam Pract. 2006;55(2):106-12. 3. Kim GK. The risk of fluoroquinolone-induced tendinopathy and tendon rupture: what does the clinician needs to know? J Clin Aesthet Dermatol. 2010;3(4):49-54. 4. Smith K, Leyden J. Safety of doxycycline and minocycline: a systematic review. Clin Ther. 2005;27(9):1329-42. 5. Dursun D, Kim MC, Solomon A, et al. Treatment of recalcitrant recurrent corneal erosions with inhibitors of matrix metalloproteinase-9, doxycycline and corticosteroids. Am J Ophthalmol. 2001;132:8-13. 6. Wang, L, Tsang H, Coroneo M. Treatment of recurrent corneal erosion syndrome using the combination of oral doxycycline and topical corticosteroid. Clin Exp Ophthalmol. 2008;36(1):8-12. 7. Liu C, Bayer A, Cosgrove S, et al. Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011;52(3):e18-e55. 8. Shen MC, Lin HH, Lee SS, et al. Double-blind, randomized, acyclovir-controlled, parallel-group trial comparing the safety and efficacy of famciclovir and acyclovir in patients with uncomplicated herpes zoster. J Microbiol Immunol Infect. 2004;37(2):75-81. 9. Severson E, Baratz K, Hodge D, Burke J. Herpes zoster ophthalmicus in olmsted county, Minnesota: have systemic antivirals made a difference. Arch Ophthalmol. 2003;121:386-90. 10. Alper BS, Lewis PR. Does treatment of acute herpes zoster prevent or shorten postherpetic neuralgia? J Fam Pract. 2000;49(3):255-64. 11. Cobo M, Foulks GN, Liesegang T, et al. Observations on the natural history of herpes zoster ophthalmicus. Curr Eye Res. 1987;6:195-9. 12. Schwartz GS, Holland EJ. Oral acyclovir for the management of herpes simplex virus keratitis in children. Ophthalmology. 2000;107(2):278-82. 13. Acyclovir for the prevention of recurrent herpes simplex virus eye disease. Herpetic Eye Disease Study Group. N Engl J Med. 1998;339(5):300-6. 14. Miserocchi E, Modorati G, Galli L, et al. Efficacy of valacyclovir vs acyclovir for the prevention of recurrent herpes simplex virus eye disease: a pilot study. Am J Ophthalmol. 2007;144(4):547-51. 15. Murakami S, Mutsuhiko M, Nakashiro Y, et al. Bell palsy and herpes simplex virus: identification of viral DNA in endoneurial fluid and muscle. Annals of Internal Medicine. 1996;124(1):27-30. 16. Adour KK, Bell DN, Hilsinger RL. Herpes simplex virus in idiopathic facial paralysis (Bell palsy). JAMA. 1975;233(6):527-30. 17. Adour KK, Ruboyianes JM, Von Doersten PG, et al. Bell’s palsy treatment with acyclovir and prednisone compared with prednisone alone: a double-blind, randomized, controlled trial. Ann Otol Rhinol Laryngol. 1996;105(5):371-8. |
