 |
10 Questions on Digital Devices and Eye Health—Answered!
With screen time rising in children and adults, ODs must understand the potential impact.
By Lisa Ostrin, OD, PhD
Release Date: January 15, 2022
Expiration Date: January 15, 2025
Estimated Time to Complete Activity: 2 hours
Jointly provided by Postgraduate Institute for Medicine (PIM) and Review Education Group
Educational Objectives: After completing this activity, the participant should be better able to:
- Discuss blue light exposure.
- Recognize the potential risks associated with blue light exposure.
- Describe the effect blue light has on circadian rhythms and sleep status.
- Educate patients on the impact blue light can have on eye health.
Target Audience: This activity is intended for optometrists engaged in managing patients who present with blue light-related ocular problems.
Accreditation Statement: In support of improving patient care, this activity has been planned and implemented by the Postgraduate Institute for Medicine and Review Education Group. Postgraduate Institute for Medicine is jointly accredited by the Accreditation Council for Continuing Medical Education, the Accreditation Council for Pharmacy Education, and the American Nurses Credentialing Center, to provide continuing education for the healthcare team. Postgraduate Institute for Medicine is accredited by COPE to provide continuing education to optometrists.
Reviewed by: Salus University, Elkins Park, PA
Faculty/Editorial Board: Lisa Ostrin, OD, PhD
Credit Statement: This course is COPE approved for 2 hours of CE credit. Activity #123115 and course ID 76185-GO. Check with your local state licensing board to see if this counts toward your CE requirement for relicensure.
Disclosure Statements:
Author: Dr. Ostrin has no financial interests to disclose.
Managers and Editorial Staff: The PIM planners and managers have nothing to disclose. The Review Education Group planners, managers and editorial staff have nothing to disclose.
With significant increases in daily screen time, the impact of such exposure on eye health, and from blue light exposure in particular, has gained increased interest in recent years. Numerous questions surround the potential implications of digital device use on eye health. In this article, the effects of digital device use specific to the eye will be discussed, as well as the role of the optometrist in educating patients on the risks of digital device exposure and mitigation strategies.
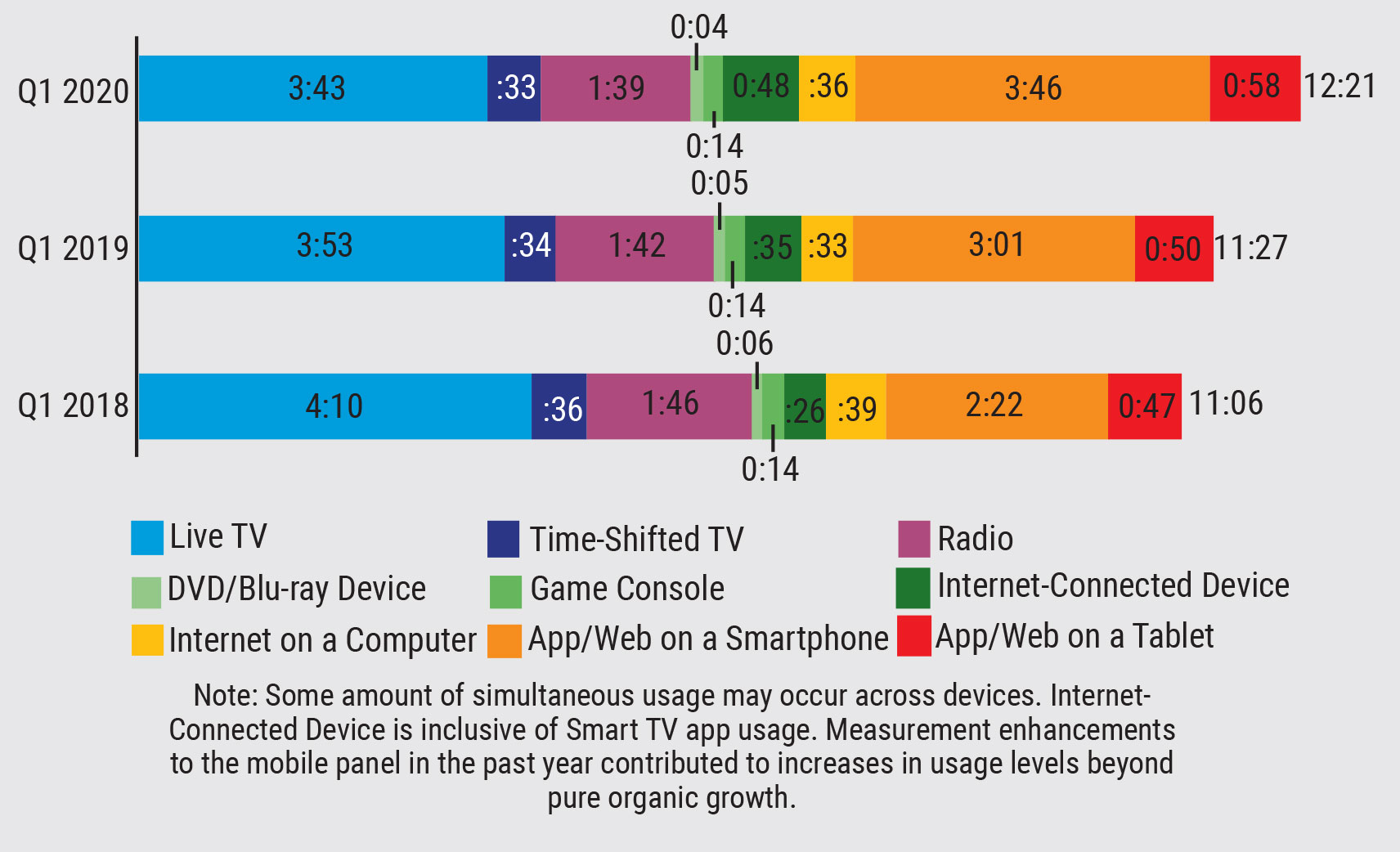 |
| Fig. 1. Average daily time spent on screens for adults 18 years and older.1 Click to enlarge. |
How Much Screen Time Are We Getting?
Digital devices are increasingly used by children and adults for education, gaming, social interaction and other daily activities, such as shopping. It was estimated that adults 18 years and older spent an average of 12 hours and 21 minutes per day using screens in the first quarter of 2020 (Figure 1).1 Children ages 10 to 18 years spent 12 hours per day on average using electronic devices during the 2021 school year.2 In the United States, 44% of children use mobile devices before the age of one, and by age four, 75% have their own mobile device.3
What is Blue Light?
Before discussing blue light in the context of digital devices, let’s discuss light as electromagnetic radiation (Figure 2). Light that is perceived by the human eye is termed “visible light,” which ranges from approximately 400nm to 700nm. Wavelengths from 400nm to 500nm are generally perceived as “blue,” medium wavelengths from 500nm to 600nm are perceived as “green” and longer wavelengths from 600nm to 700nm are perceived as “red.” Short-wavelength blue light has higher energy than long-wavelength red light.
Ultraviolet (UV) light includes wavelengths that are shorter than visible light, ranging from approximately 10nm to 400nm, and infrared light includes wavelengths that are longer than visible light, from approximately 700nm to 1mm. The majority of UV light that reaches the eye is absorbed by the cornea, which absorbs UV-C, and the crystalline lens, which absorbs UV-A, -B and -C, and therefore does not reach the retina.
An additional protection from light damage is the macular pigment, consisting of zeaxanthin and lutein, which absorbs approximately 40% of high-energy blue light with an absorption spectrum peaking at 460nm.4
The spectral output (i.e., wavelength composition) is comprised of various natural and artificial sources of light (Figure 3). The highest intensity light that humans are exposed to is sunlight, which can be as high as 150,000 lux on a bright sunny day. Indoor room illuminance generally ranges from 30 to 600 lux, and illuminance from electronic devices is in the range of 40 to 300 lux.5,6
Sunlight is made up of all wavelengths of the electromagnetic spectrum and represents the greatest source of light that humans are exposed to, including blue light, red light and all wavelengths in between. Fluorescent lights provide broadband illumination, with peaks across the entire visible spectrum. Incandescent lights lean toward longer wavelengths, appearing more orange-red, and traditional white-light LEDs (the most common type of LED) peak in the short wavelength region, thereby emitting a higher proportion of blue light. Electronic devices, including televisions, computer monitors, tablets and smartphones, are typically backlit by LEDs and therefore emit blue light.
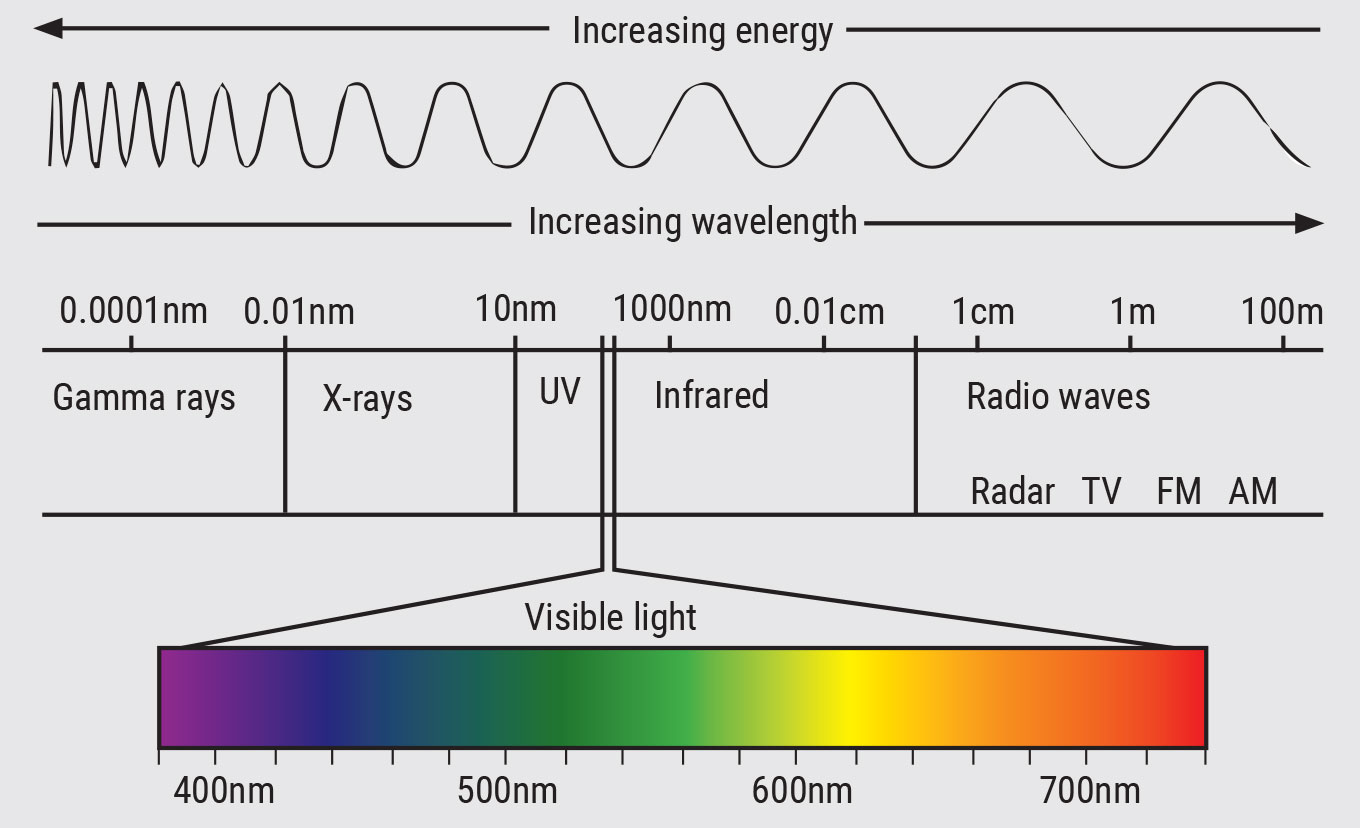 |
| Fig. 2. The electromagnetic spectrum. Adapted from Cyberphysics. Click to enlarge. |
Why Do We Need Blue Light?
Light is the most important cue for entraining circadian rhythm. These rhythms represent the fluctuations in physiological processes over the course of approximately 24 hours. They are controlled both by light exposure and endogenous molecular clocks.
Light information is conveyed from the eye to the suprachiasmatic nucleus by the intrinsically photosensitive retinal ganglion cells (ipRGCs), which are light-sensitive ganglion cells in the inner retina that contain the photopigment melanopsin.7 Melanopsin is most sensitive to short-wavelength blue light of approximately 480nm. The ipRGCs also convey light information from the rod/cone pathways.
Light exposure, and particularly melanopsin-activating blue light exposure, signals to the body that it is daytime. In the dark, ipRGC signaling decreases and melatonin is secreted. Melatonin, the sleep hormone, undergoes a sharp rise in response to dim light approximately one to three hours before bedtime, known as dim light melatonin onset. Exposure to regular light/dark patterns, i.e., light during the day and darkness at night, is critical for overall health and performance. A growing body of evidence shows that the timing, intensity, spectral composition and duration of light exposure all contribute to circadian health.8,9
What Are the Potential Effects of Blue Light On the Eye?
Much of the concern regarding blue light stems from early studies showing that light can damage the retinas of rats and rhesus monkeys.10-12 One found that prolonged exposure to fluorescent light (wavelengths of 490nm to 580nm) caused phototoxic damage in albino rats.10 Another found that a laser of 441nm directed at the retinas of anesthetized monkeys at 33 J/cm2 resulted in clumping and phagocytosis of melanin that could be observed histologically as focal lesions.12 After converting these laboratory thresholds into solar energy values, it was concluded that “sungazing at bright midnoon for 100 seconds can produce a threshold lesion.”12
Several studies have investigated the effects of blue light on the human retina. One showed that isolated human retinal pigment epithelial (RPE) cells were injured with exposure to blue light of 400nm, while exposure to 420nm and 435nm did not cause cellular damage.13 Another found that short wavelengths (390nm to 450nm) led to lipofuscin photoreactivity in cultured human RPE cells.14 Blue light-induced damage and death of isolated RPE cells is caused by mitochondria-derived reactive oxygen species.15 However, blue light exposure in these laboratory studies was of high intensity and long duration, presented directly to retinal cells and without the filtering properties of the ocular media that is present in a human eye.
Findings such as these, and those in animals, have led to the concept of “blue light hazard,” raising concern that prolonged exposure to blue light-emitting devices can damage the retina and cause age-related macular degeneration (AMD) (Figure 4).
Numerous studies have investigated whether sunlight increases the risk of AMD but have found inconsistent results.16-20 In a study of watermen aged 65 and older, those with advanced AMD had significantly higher exposure to blue or visible light in the previous 20 years. However, there was no association between mild to moderate AMD and blue or visible light.
The Beaver Dam Eye Study reported an associated between extended exposure to summer sun and the 10-year incidence of early AMD and macular pigment.16 On the other hand, a 2018 meta-analysis of 14 studies concluded that sunlight exposure may not be associated with increased risk of AMD.21 The absence of a clear association between sunlight exposure and AMD means that light emitted from digital devices, at exponentially lower levels, may present no risk of AMD.
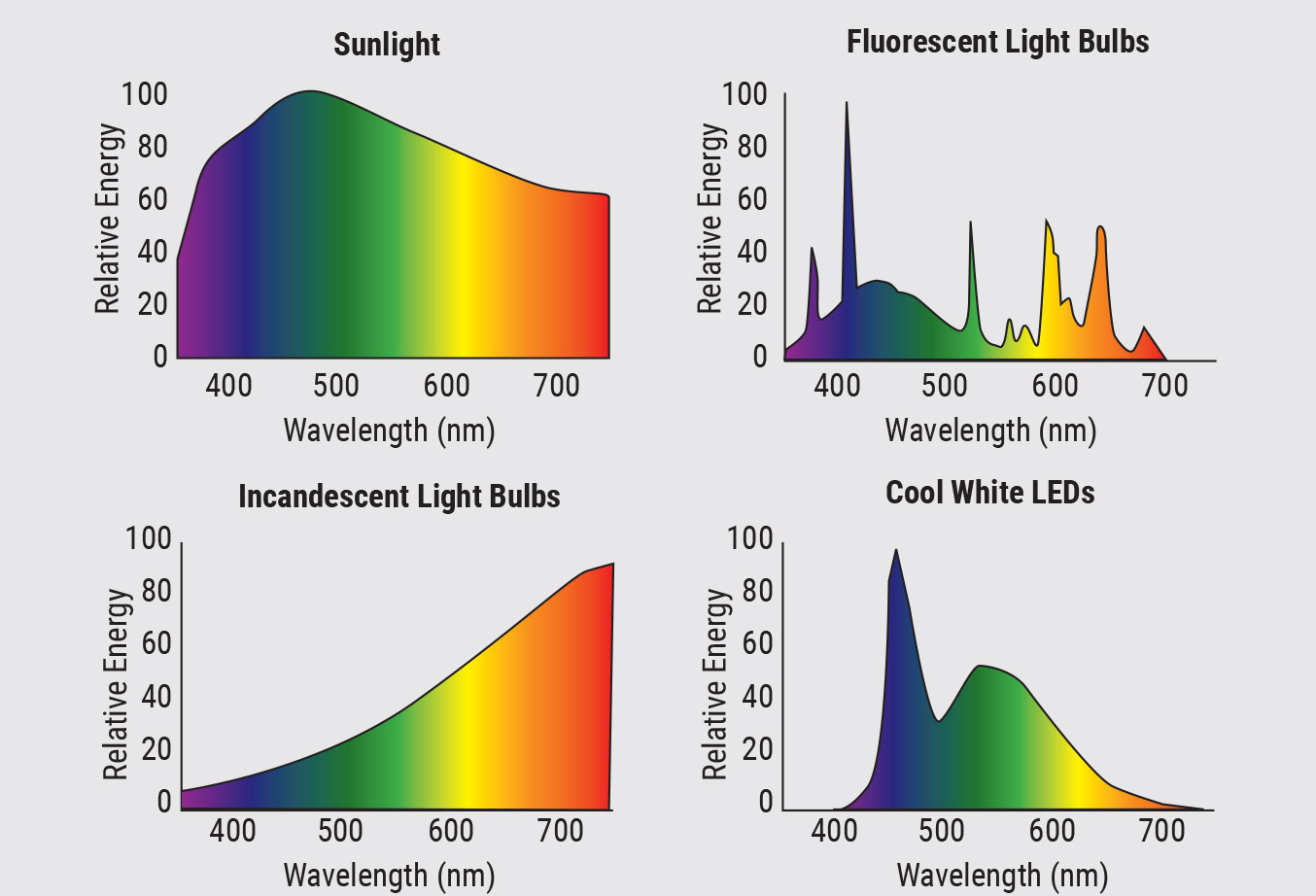 |
| Fig. 3. Spectral composition of sunlight, fluorescent light bulbs, incandescent light bulbs and cool white LEDs. Click to enlarge. |
What Are Blue-Blocking Lenses?
These are ophthalmic lenses that filter light within the 400nm to 500nm range. Traditionally, spectacle lenses, contact lenses and intraocular lenses are designed to block UV light. The integration of a yellow chromophore blocks wavelengths in the blue portion of the visible spectrum, and additional coatings on the anterior and/or posterior surface of the lens can selectively filter wavelengths in the blue-violet light spectrum (415nm to 455nm). Blue-blocking lenses are widely marketed to relieve “hazardous blue light” exposure and digital eye strain.
Blue-blocking lenses are variable in the proportion of blue light that is filtered, ranging from 10% to 100%. In one study, researchers measured the transmittance of seven commercially available blue-blocking lenses.22 They found that while all of the lenses blocked 100% of the UV light less than 400nm, transmittance in the blue range varied widely (Figure 5). On average, blue-blocking lenses filter 5% to 40% of the blue wavelengths. To reach greater filtering, the lenses will generally be tinted yellow or amber.
Can Blue Light From Digital Devices Lead to Retinal Damage?
International standards for blue light exposure were developed based on early studies.23 One investigated the level of blue light emitted from digital devices with respect to international standards and the blue light hazard.24 The authors tested numerous computer monitors, laptops, tablets and smartphones and calculated that all devices were within 0.03% to 0.38% of the blue light exposure limit threshold, concluding that these devices do not represent a hazard to the human retina, even during prolonged viewing. In other words, it is extremely unlikely that any patient is exposed to blue light outside of the safe range, regardless of their screen time.
What is the Link Between Digital Device Use and Eye Strain?
Digital eye strain, also known as computer vision syndrome, refers to a group of eye- and vision-related symptoms that result from extended use of screens, including computers, tablets, e-readers and smartphones.25 Digital eye strain has become increasingly prevalent, with studies reporting that up to 40% of office workers and 80% of children experience symptoms, some of which may significantly impact productivity.26-28
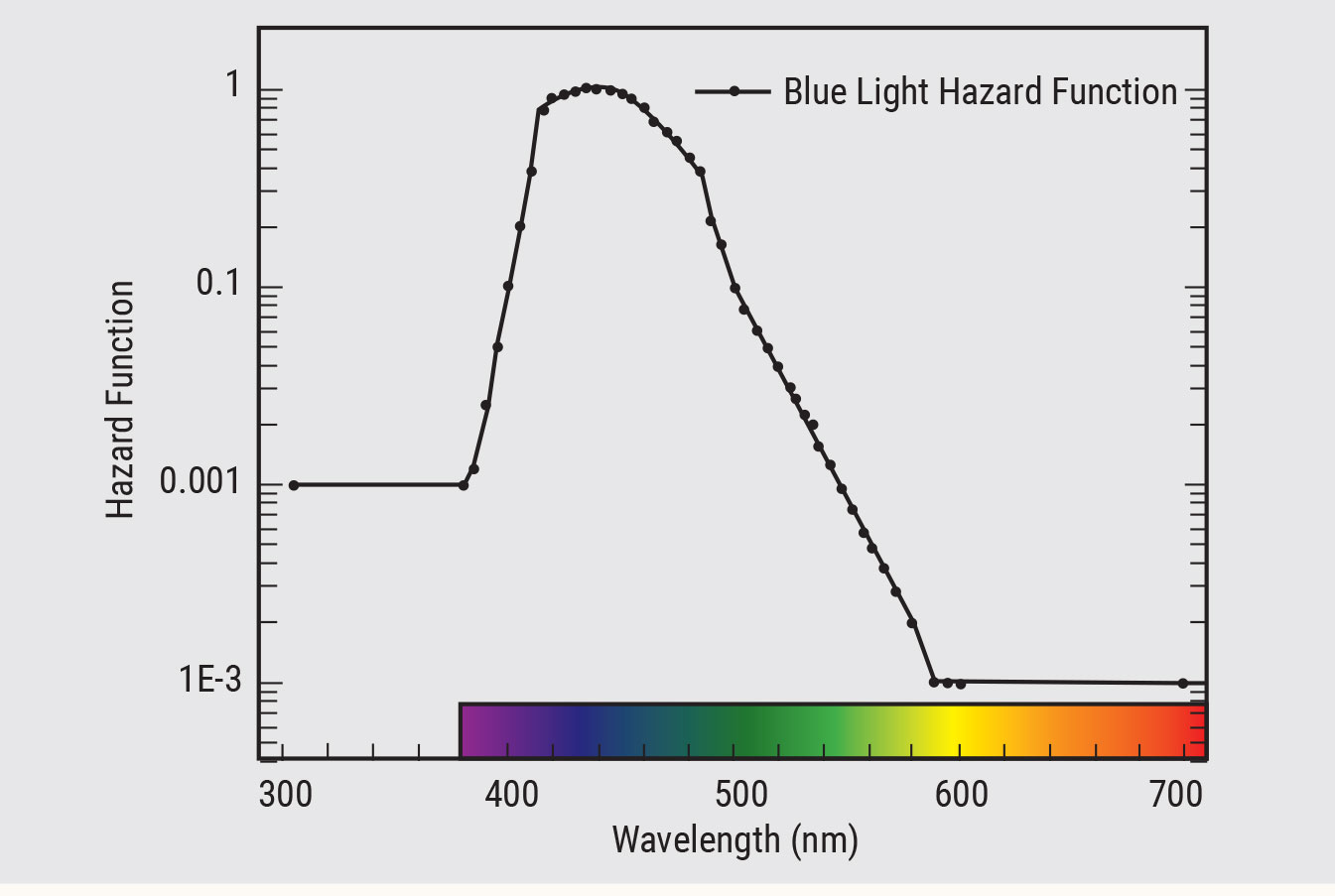 |
| Fig. 4. Blue light hazard function.56 Click to enlarge. |
Digital eye strain includes two broad categories of symptoms: those linked to binocular or accommodative stress and those linked to dry eye. The most common symptoms beside eye strain include headache, blurred vision, dry eye and pain in the neck and shoulders. Dry eye can affect both adults and children and may cause a decreased blink rate or incomplete blinks with digital device use.29-38
Many manufacturers market blue-blocking lenses to reduce symptoms of digital eye strain. However, there is little evidence to support the claim that blue light in particular is the cause of digital eye strain. Additionally, there are no physiological mechanisms that link blue light exposure to symptoms of digital eye strain.
One study measured critical fusion frequency following a two-hour computer task with and without blue-blocking lenses.29 Critical fusion frequency is a metric representing fatigue and mental workload.30 Findings showed that wearing a filter that blocked approximately 60% of blue light resulted in the greatest change in critical fusion frequency, which the authors interpreted as less fatigue, compared with wearing a filter that blocked 24% or 3% of blue light. However, when analyzing the proportion of subjects in each group showing a post-task symptomatic improvement for each question, a significant improvement with the blue-filtering lens was only found for one question, “My eyes feel itchy.”
A more recent study examined symptoms of digital eye strain when participants wore a lens that blocked 99% of blue light compared with an equivalent neutral density filter.39 Findings showed that the blue-blocking filter was no more effective at reducing symptoms of digital eye strain than the neutral density filter.
Two other double-blind studies on symptoms of digital eye strain also showed no improvement with the blue-blocking lenses, and a recent review concluded that there were no significant differences in relation to the proportion of subjects showing an improvement in symptoms of eye strain or eye fatigue between blue-blocking and control spectacle lenses.29,31-33,40
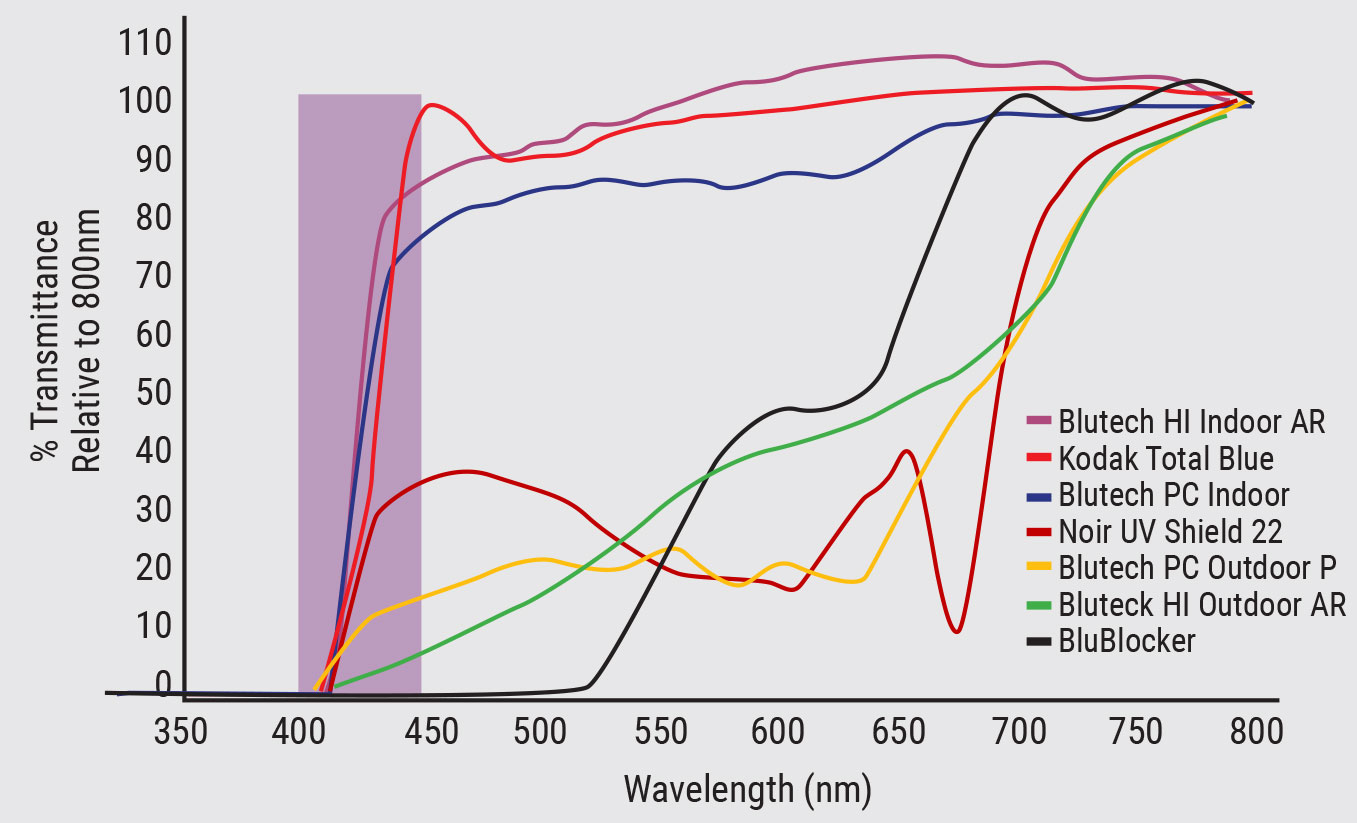 |
| Fig. 5. Transmission spectrum of seven commercially available blue-blocking lenses.22 Click to enlarge. |
How Does Digital Device Use Impact Sleep?
Nighttime use of electronic devices, including televisions, computers and handheld devices, is highly prevalent, with 90% of Americans reporting electronic device use in the hour before bedtime.41 Evening exposure to short-wavelength light prior to bedtime may disrupt sleep through ipRGC-induced melatonin suppression, contributing to the high frequency of reported cases of sleep dysfunction, which affects up to 40% of the population.42-45 Computers, cell phones and video games at night are associated with more difficulty falling asleep and less restful sleep.41 Evening smartphone use, with and without a blue-blocking filter, showed attenuated nighttime melatonin in comparison with reading a printed book, albeit less so when the filter was used.46
An obvious solution to combat light-induced melatonin suppression is to cease electronic device use and dim indoor artificial lights a few hours before bedtime. However, given challenging academic obligations and demanding workloads, this is often an unrealistic expectation. An alternative is the use of blue-blocking lenses before bedtime.
A recent study showed that wearing blue-blocking glasses before bedtime, even while continuing to work on digital devices, increased nighttime melatonin by 58%, increased sleep duration by 24 minutes and improved subjective sleep quality.47 Note that the lenses used in that study blocked nearly 100% of wavelengths less than 500nm and were worn only at bedtime, not throughout the day. Another study demonstrated subjective improvements in both sleep quality and mood, as well as a decrease in LED-induced nighttime melatonin suppression, in participants wearing blue-blocking glasses at nighttime for two weeks.48,49
What is the Connection Between Digital Device Use and Myopia?
A common concern for parents is whether digital devices contribute to myopia. The prevalence of myopia is increasing faster than genetics can account for, and it is well accepted that there are environmental and behavioral contributions to myopia. Not only is the prevalence of myopia increasing, but the age of onset is also younger, progression is accelerated and high myopia is increasing.50 These observations raise the question of whether screen time contributes to myopia.
 |
| Fig. 6. Screen exposure may have a negative effect on ocular surface health. Photo: Getty Images. Click to enlarge. |
Two major risk factors associated with myopia are decreased time outdoors and increased near work. Screen time represents a form of near work. Children use digital devices for long durations, often uninterrupted, and at a close distance. Studies show that children typically view handheld devices from distances of approximately 10cm to 30cm (Figure 6).51 Additionally, it is likely that if children spend increased time on digital devices, they are spending less time outdoors.
Studies examining the association between screen time and myopia are conflicting. Some reveal a link between screen time and myopia, reporting more screen time is associated with a higher prevalence of myopia, increased myopic refraction and longer axial length.52 However, others have found no link between the two.53,54
A systematic review published in 2020 included five studies and found no association between prevalent or incident myopia and digital screen time.55 Another systematic review and meta-analysis published in 2021 (33 articles and 11 articles, respectively) reported a weighted odds ratio of 1.26 from cross-sectional and prospective studies. The authors of the review article concluded that there is insufficient and conflicting literature on the association between digital device use and myopia.
Investigating the relationship between device use and myopia is challenging for many reasons. It is difficult to investigate device use as an independent factor, separate from near work. Additionally, device use is generally estimated from parent questionnaires, which are inherently confounded by recall errors and biases. Many studies have included Asian populations and may not be generalizable. Importantly, associations between screen time and myopia reported in observational studies do not infer causal relationships.
What is the Optometrist’s Role?
Many patients are concerned about “blue light hazard,” in part due to extensive marketing of blue-blocking lenses. It is the optometrist’s obligation to educate their patients and present evidence-based clinical recommendations. Patients should be informed that there are no physiological mechanisms linking blue light to digital eye strain, that blue-blocking lenses show no benefit to eye comfort in controlled clinical trials and that there is no evidence supporting a link between digital device use and retinal damage. Additionally, patients should be notified that studies investigating links between screen time and myopia are conflicting and inconclusive.
Optometrists should educate parents that nighttime screen time and artificial light can lead to sleep disruptions. They can also convey general recommendations for screen use in children by referring parents to guidelines set by the American Academy of Pediatricians and World Health Organization.
How can the OD help relieve digital eye strain? Note that it is a diagnosis of exclusion. Refractive status must be comprehensively examined, considering objective and subjective as well as non-cyclopleged and cyclopleged measures. A careful assessment of binocular vision should be performed, as binocular vision conditions can often present with the same symptoms as digital eye strain. A patient’s individual viewing needs should be discussed, which will vary based on academic or work demands and leisure screen time. Patients who are presbyopic or nearing presbyopia, or those with reduced accommodative amplitude and facility, may benefit from computer glasses to reduce accommodative demand at their habitual computer-viewing distance.
Physical attributes, such as body height and arm length, should be considered. For both children and adults, workstations should be set up with ideal ergonomics that take into account viewing distance, angle and height. Glare, brightness, contrast and font size are also important factors for comfort during extended screen time. Dry eye symptoms related to digital devices can be addressed by teaching the patient to blink during screen time, using lubricating drops and employing other traditional treatments for dry eye. A common clinical recommendation is the 20-20-20 rule. For every 20 minutes of near work, look at objects further than 20 feet away for at least 20 seconds. This general rule-of-thumb may help remind patients to blink and intermittently relax their eyes.
Based on studies demonstrating the attenuating effects of blue light on melatonin, screen time and artificial light exposure should be decreased one to two hours before bedtime.46,47 This can also be accomplished through the use of amber-tinted lenses before bedtime. Lenses with the ability to block close to 100% of shorter wavelengths are the most effective. Other options include using apps and installing home lighting that both aim to reduce blue light.
Dr. Ostrin is an associate professor at the University of Houston College of Optometry, where she received her optometry degree and PhD. She teaches in the optometry and vision science programs, covering topics such as gross anatomy, ocular anatomy, eye growth and accommodation. She is a fellow of the American Academy of Optometry and a gold fellow of the Association for Research in Vision and Ophthalmology. She has no relevant financial interests to disclose.
1. Staying PUT: consumers forced indoors during crisis spend more time on media. 2020. www.nielsen.com/us/en/insights/article/2020/staying-put-consumers-forced-indoors-during-crisis-spend-more-time-on-media. Accessed November 20, 2021. 2. Bhandari K, Shukla D, Mirhajianmoghadam H, et al. Objectively measured habitual viewing behaviors in schoolchildren. Optom Vis Sci Suppl. 2021;E-Abstract 215133. 3. Kabali HK, Irigoyen MM, Nunez-Davis R, et al. Exposure and use of mobile media devices by young children. Pediatrics. 2015;136(6):1044-50. 4. Loane E, Kelliher C, Beatty S, et al. The rationale and evidence base for a protective role of macular pigment in age-related maculopathy. Br J Ophthalmol. 2008;92(9):1163-8. 5. Gringas P, Middleton B, Skene D, et al. Bigger, brighter, bluer-better? Current light-emitting devices-adverse sleep properties and preventative strategies. Front Public Health. 2015;3:233. 6. Ostrin LA. Objectively measured light exposure in emmetropic and myopic adults. Optom Vis Sci. 2017;94(2):229-38. 7. Sollars PJ, Smeraski CA, Kaufman JD, et al. Melanopsin and non-melanopsin expressing retinal ganglion cells innervate the hypothalamic suprachiasmatic nucleus. Vis Neurosci. 2003;20(6):601-10. 8. Bumgarner JR, Nelson RJ. Light at night and disrupted circadian rhythms alter physiology and behavior. Integr Comp Biol. 2021;61(3):1160-9. 9. Xiao H, Cai H, Li X. Non-visual effects of indoor light environment on humans: a review. Physiol Behav. 2021;228:113195. 10. Noell WK, Walker VS, Kang BS, et al. Retinal damage by light in rats. Invest Ophthalmol. 1966;5(5):450-73. 11. Ham WT Jr., Ruffolo JJ Jr., Mueller HA, et al. Histologic analysis of photochemical lesions produced in rhesus retina by short-wave-length light. Invest Ophthalmol Vis Sci. 1978;17(10):1029-35. 12. Ham WT Jr., Mueller HA, Sliney DH. Retinal sensitivity to damage from short wavelength light. Nature. 1976;260(5547):153-5. 13. Youn HY, Chou BR, Cullen AP, et al. Effects of 400 nm, 420 nm, and 435.8 nm radiations on cultured human retinal pigment epithelial cells. J Photochem Photobiol B. 2009;95(1):64-70. 14. Davies S, Elliott MH, Floor E, et al. Photocytotoxicity of lipofuscin in human retinal pigment epithelial cells. Free Radic Biol Med. 2001;31(2):256-65. 15. King A, Gottlieb E, Brooks DG, et al. Mitochondria-derived reactive oxygen species mediate blue light-induced death of retinal pigment epithelial cells. Photochem Photobiol. 2004;79(5):470-5. 16. Tomany SC, Cruickshanks KJ, Klein R, et al. Sunlight and the 10-year incidence of age-related maculopathy: the Beaver Dam Eye Study. Arch Ophthalmol. 2004;122(5):750-7. 17. Taylor HR, West S, Munoz B, et al. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992;110(1):99-104. 18. Darzins P, Mitchell P, Heller RF. Sun exposure and age-related macular degeneration. An Australian case-control study. Ophthalmology. 1997;104(5):770-6. 19. Mitchell P, Smith W, Wang JJ. Iris color, skin sun sensitivity, and age-related maculopathy. The Blue Mountains Eye Study. Ophthalmology. 1998;105(8):1359-63. 20. Delcourt C, Carriere I, Ponton-Sanchez A, et al. Light exposure and the risk of age-related macular degeneration: the Pathologies Oculaires Liees a l’Age (POLA) study. Arch Ophthalmol. 2001;119(10):1463-8. 21. Zhou H, Zhang H, Yu A, et al. Association between sunlight exposure and risk of age-related macular degeneration: a meta-analysis. BMC Ophthalmol. 2018;18(1):331. 22. Giannos SA, Kraft ER, Lyons LJ, et al. Spectral evaluation of eyeglass blocking efficiency of ultraviolet/high-energy visible blue light for ocular protection. Optom Vis Sci. 2019;96(7):513-22. 23. Protection ICoN-IR. ICNIRP guidelines on limits of exposure to incoherent visible and infrared radiation. Health Physics. 2013;105:23. 24. O’Hagan JB, Khazova M, Price LL. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye. 2016;30(2):230-3. 25. Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31(5):502-15. 26. Portello JK, Rosenfield M, Bababekova Y, et al. Computer-related visual symptoms in office workers. Ophthalmic Physiol Opt. 2012;32(5):375-82. 27. The 21st Century Eye: Three Ways to Protect Your Vision [press release]. aoa.org. 2015. 28. Daum KM, Clore KA, Simms SS, et al. Productivity associated with visual status of computer users. Optometry. 2004;75(1):33-47. 29. Lin JB, Gerratt BW, Bassi CJ, et al. Short-wavelength light-blocking eyeglasses attenuate symptoms of eye fatigue. Invest Ophthalmol Vis Sci. 2017;58(1):442-7. 30. Luczak A, Sobolewski A. Longitudinal changes in critical flicker fusion frequency: an indicator of human workload. Ergonomics. 2005;48(15):1770-92. 31. Singh S, Downie LE, Anderson AJ. Do blue-blocking lenses reduce eye strain from extended screen time? A double-masked randomized controlled trial. Am J Ophthalmol. 2021;226:243-51. 32. Rosenfield M, Li RT, Kirsch NT. A double-blind test of blue-blocking filters on symptoms of digital eye strain. Work. 2020;65(2):343-8. 33. Leung TW, Li RW, Kee CS. Blue-light filtering spectacle lenses: optical and clinical performances. PloS one. 2017;12(1):e0169114. 34. Courtin R, Pereira B, Naughton G, et al. Prevalence of dry eye disease in visual display terminal workers: a systematic review and meta-analysis. BMJ Open. 2016;6(1):e009675. 35. Moon JH, Lee MY, Moon NJ. Association between video display terminal use and dry eye disease in school children. J Ped Ophthalmol Strab. 2014;51(2):87-92. 36. Patel S, Henderson R, Bradley L, et al. Effect of visual display unit use on blink rate and tear stability. Optom Vis Sci. 1991;68(11):888-92. 37. Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med. 1993;328(8):584. 38. Chu CA, Rosenfield M, Portello JK. Blink patterns: reading from a computer screen versus hard copy. Optom Vis Sci. 2014;91(3):297-302. 39. Palavets T, Rosenfield M. Blue-blocking filters and digital eyestrain. Optom Vis Sci. 2019;96(1):48-54. 40. Lawrenson JG, Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: a systematic review of the literature. Ophthalmic Physiol Opt. 2017;37(6):644-54. 41. Gradisar M, Wolfson AR, Harvey AG, et al. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. J Clin Sleep Med. 2013;9(12):1291-9. 42. Vartanian GV, Li BY, Chervenak AP, et al. Melatonin suppression by light in humans is more sensitive than previously reported. J Biol Rhythms. 30(4):351-4. 43. Brainard GC, Hanifin JP, Warfield B, et al. Short-wavelength enrichment of polychromatic light enhances human melatonin suppression potency. J Pineal Res. 2015;58(3):352-61. 44. Mai E, Buysse DJ. Insomnia: prevalence, impact, pathogenesis, differential diagnosis, and evaluation. Sleep Med Clin. 2008;3(2):167-74. 45. Mottram AR, Svenson JE. Rhythm disturbances. Emerg Med Clin North Am. 2011;29(4):729-46. 46. Schmid SR, Hohn C, Bothe K, et al. How smart is it to go to bed with the phone? The impact of short-wavelength light and affective states on sleep and circadian rhythms. Clocks Sleep. 2021;3(4):558-80. 47. Ostrin LA, Abbott KS, Queener HM. Attenuation of short wavelengths alters sleep and the ipRGC pupil response. Ophthalmic Physiol Opt. 2017;37(4):440-50. 48. Burkhart K, Phelps JR. Amber lenses to block blue light and improve sleep: a randomized trial. Chronobiol Int. 2009;26(8):1602-12. 49. van der Lely S, Frey S, Garbazza C, et al. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J Adolesc Health. 2015;56(1):113-9. 50. Chua SY, Sabanayagam C, Cheung YB, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36(4):388-94. 51. Bhandari KR, Ostrin LA. Objective measures of viewing behaviour in children during near tasks. Clin Exp Optom. 2021:1-8. 52. Hansen MH, Laigaard PP, Olsen EM, et al. Low physical activity and higher use of screen devices are associated with myopia at the age of 16-17 years in the CCC2000 Eye Study. Acta Ophthalmol. 2020;98(3):315-21. 53. Hagen LA, Gjelle JVB, Arnegard S, et al. Prevalence and Possible Factors of Myopia in Norwegian Adolescents. Sci Rep. 2018;8(1):13479. 54. Toh SH, Coenen P, Howie EK, et al. A prospective longitudinal study of mobile touch screen device use and musculoskeletal symptoms and visual health in adolescents. Appl Ergon. 2020;85:103028. 55. Lanca C, Saw SM. The association between digital screen time and myopia: a systematic review. Ophthalmic Physiol Opt. 2020;40(2):216-29. 56. Price RB, Labrie D, Bruzell EM, et al. The dental curing light: a potential health risk. J Occup Environ Hyg. 2016;13(8):639-46. |
